Definition and prevalence rate of pressure ulcers
As defined by the European Pressure Ulcer Advisory Panel (EPUAP), National Pressure Ulcer Advisory Panel (NPUAP) and Pan Pacific Pressure Injury Alliance (PPPIA), a pressure ulcer is ‘localised injury to the skin and/or underlying tissue usually over a bony prominence, as a result of pressure, or pressure in combination with shear’ (EPUAP/NPUAP/PPPIA, 2019a). They can have a substantial impact on multiple aspects of an individual’s life, including reduced quality of life, and result in higher costs for healthcare services (Demarré et al, 2015; Song et al, 2019).
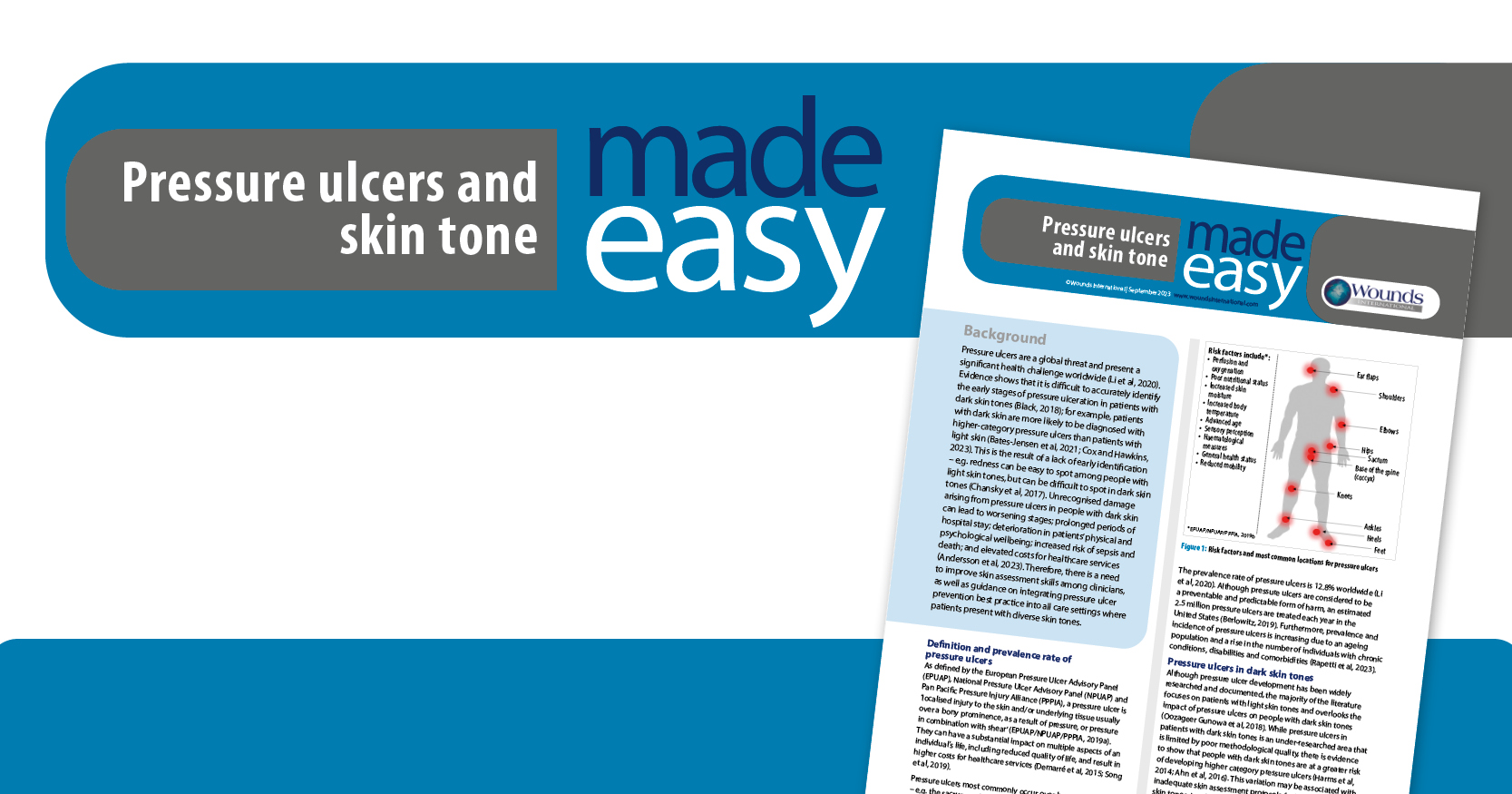
Pressure ulcers most commonly occur over bony prominences – e.g. the sacrum and heel (Borojeny et al, 2020). Pressure ulcers can affect people of any age, but they especially affect older and frail patients who may have mobility issues, which increases their risk of developing pressure ulcers (Shi et al, 2021; Andersson et al, 2023). Ultimately, pressure ulcer formation is highly influenced by a number of intrinsic and extrinsic factors (Boyko et al, 2018; Figure 1).
The prevalence rate of pressure ulcers is 12.8% worldwide (Li et al, 2020). Although pressure ulcers are considered to be a preventable and predictable form of harm, an estimated 2.5 million pressure ulcers are treated each year in the United States (Berlowitz, 2019). Furthermore, prevalence and incidence of pressure ulcers is increasing due to an ageing population and a rise in the number of individuals with chronic conditions, disabilities and comorbidities (Rapetti et al, 2023).
Pressure ulcers in dark skin tones
Although pressure ulcer development has been widely researched and documented, the majority of the literature focuses on patients with light skin tones and overlooks the impact of pressure ulcers on people with dark skin tones (Oozageer Gunowa et al, 2018). While pressure ulcers in patients with dark skin tones is an under-researched area that is limited by poor methodological quality, there is evidence to show that people with dark skin tones are at a greater risk of developing higher category pressure ulcers (Harms et al, 2014; Ahn et al, 2016). This variation may be associated with inadequate skin assessment protocols for individuals with dark skin tones. In addition, there is a significant lack of knowledge and guidance to support clinicians to identify and manage pressure ulcers in people with dark skin tones.
Clinicians should avoid using ethnicity or racial descriptors as a proxy for skin tone, as ethnic and racial background is an unreliable determinant of pressure ulcer risk (Oozageer Gunowa et al, 2018). Furthermore, it is critical that clinicians avoid using metaphors or similes when describing skin tone, such as comparing skin tones to food (e.g. cocoa and coffee).
Assessing pressure-related damage in dark skin tones
It has been acknowledged that skin tone variance may affect early detection of pressure ulcers (Dhoonmoon et al, 2021). Many of the signs and symptoms that clinicians have been educated to look for may present differently depending on the patient’s skin tone; for example, it has been found that dark skin rarely shows the blanching response that clinicians are trained to look out for, and erythema may also be hard to detect (Grimes, 2009). It is also important to remember that skin irritation in patients with dark skin tones may cause hyperpigmentation (increased pigmentation) or hypopigmentation (reduced pigmentation), with no redness visible (Nijhawan and Alexis, 2011). By the time textural changes to the skin have been detected, the damage may be more severe. Additionally, categorisation of pressure ulcers can be a major challenge in clinical practice regardless of skin tone.
In dark skin tones, it can be difficult to predict exactly what erythema will look like (Dhoonmoon et al, 2023), and this is due to high melanin concentration in the skin (Baker, 2016). In addition, it is not uncommon for dark skin to present with age-related hyperpigmentation, which can mask the visual identification of erythema. It can be suggested that people with dark skin tones face a disadvantage, as category 1 pressure ulcers are more likely to go undetected and deteriorate to full thickness pressure ulcers – e.g. category 3 and 4 (Bennet, 1995; Springle et al, 2009). Moreover, research has shown a pattern of underdiagnosis of category 1 pressure ulcers in dark skin tones (Oozageer Gunowa et al, 2018).
Traditionally, nurses have been taught to look for redness in order to detect the first signs of pressure damage (Kariwo et al, 2023). However, since initial redness can show differently on dark skin tones and, therefore, be missed in the initial assessment, clinicians need to assess for other indicators of injury and use both visual and tactile cues – e.g. purple/bluish discolouration and change in temperature [Box 1; Figure 2 A-D].
Assessing for signs and symptoms of damage other than redness is important in other areas of care as well; for example, in the case of moisture associated skin damage (MASD). Although MASD is not a direct cause of pressure ulcers, it can contribute to the weakening of the skin and elevated risk of injury from shear (Fletcher, 2020). Therefore, there is a need to stop redness from remaining the focus of pressure ulcer diagnosis. Furthermore, full use of the senses – especially touch and hearing – is valuable in the assessment of all patients [Box 2]. Clinicians need to ask the patient about their skin and listen to their perspective about what they consider to be changes to their skin – e.g. tightness, pain, swelling and changes in feeling/sensation.
Establishing baseline skin tone is an important part of the initial skin inspection and holistic wound assessment (Dhoonmoon et al, 2021). Since skin changes in people with dark skin tones fail to be observed quickly enough on a global scale, use of a validated classification tool, such as the skin tone tool (Figure 3; adapted from Ho and Robinson, 2015), should be used to promote accurate assessment and early identification of damage (Dhoonmoon et al, 2023). Skin tone can be determined by selecting the tone that most closely matches the patient’s inside upper arm, since this area generally receives little sunlight and, therefore, represents baseline colour. This is vital so that any changes to the patient’s skin can be monitored and identified early.
Risk assessment and grading
Risk assessment is an important component of clinical practice that enables quick and efficient identification of patients at risk (Fletcher, 2023). It is important to note that standard risk assessment tools for pressure ulcers often rely on visual inspection and categorisation of skin tone; however, these tools may not adequately capture the specific risk factors and characteristics of dark skin. As a result, the accuracy of risk assessment may be compromised, leading to insufficient preventative measures in patients with dark skin tones.
National Institute for Health and Care Excellence (2014) recommends that a validated risk assessment tool is used to support clinical judgement when assessing pressure ulcer risk in day-to-day practice. The most commonly used pressure ulcer risk assessment tools are the Braden, Norton and Waterlow scales (Norton et al 1962; Waterlow et al, 1985; Braden and Bergstrom, 1987; Hotaling and Black, 2021). In addition, the Pressure Ulcer Risk Primary or Secondary Evaluation Tool (PURPOSE-T) is an evidence-based risk assessment tool that was developed using robust research methods. In comparison to the modified Norton scale and the Braden scale, PURPOSE-T identifies more patients at risk of pressure ulcers (Hultin et al, 2020).
Pressure ulcer severity is generally classified using an international classification system that was developed by EPUAP/NPUAP/PPPIA (2019b; Box 3). However, it is important to note that categorisation does not always indicate degree of harm. In addition, the international classification system does not currently incorporate skin tone. Once a pressure ulcer is confirmed, clinicians should report the pressure ulcer via a dedicated local incident reporting system, such as Datix. However, there is a need for pressure ulcer reporting systems to consider differences in skin tone. Any damage needs to be documented in the patient’s electronic record, to facilitate high-quality healthcare delivery and prevent pressure ulcer occurrence (Andersson et al, 2023). Systems, such as the Patient Safety Incident Response Framework (PSIRF) used in the UK, can also help clinicians to report patient safety incidents, and the framework can be used to identify trends and areas for improvement.
Pressure ulcer prevention strategies
There is evidence to show that there are differences in staff knowledge around pressure ulcers (Gunningberg et al, 2017). Zaidi (2017) concluded that it is necessary for clinicians to have sufficient knowledge of differences in culture and habits, in order to promote accuracy in diagnosis and treatment. In situations where early detection of pressure ulcers is missed, or a pressure ulcer has progressed, treatment decisions should be based on assessment, routine skin inspection, risk categorisation, treatment goals and patient preferences (Phelps et al, 2021). It is widely acknowledged that there is an underrepresentation of diverse skin tones in education on all skin conditions, including pressure ulcers, and there is an ongoing need for the inclusion of dark skin tones in case studies and photographs, to address the gap in bias around light skin tones and lack of understanding of how to assess different skin tones.
Early identification and diagnosis of changes to the skin is the most important measure to protect individuals at risk of developing pressure ulcers (EPUAP/NPUAP/PPPIA, 2019a), and clinicians need to refer to international clinical practice guidelines for the prevention and treatment of pressure ulcers (EPUAP/NPUAP/PPPIA, 2019b). In particular, education of patients and their families has been shown to sustain a reduction in pressure ulcers (Andersson et al, 2023). Clinicians should communicate with patients about good skin care (e.g. moisturising) and encourage them to check their own skin, and alert the clinician of any signs of change. Clinicians also need to encourage patients to make healthier lifestyle choices to prevent a worsening of their health condition – e.g. stop smoking, eat well and drink plenty of water.
Care bundles have been proposed as an effective way to ensure care delivered to patients in the UK is consistent, and to reduce the occurrence of complications. A recent audit of pressure ulcer prevalence (Stephenson et al, 2021) identified several key areas of care that require improvement, including patient education, keeping patients moving and regular repositioning. During the audit, adherence to elements of the ‘aSSKINg’ (assess risk, skin assessment and skin care, surface, keep moving, incontinence and moisture, nutrition and hydration, and giving information or getting help) model were investigated, which is a framework developed by the NHS as an approach to pressure ulcer prevention.
In the UK, the National Wound Care Strategy Programme (NWCSP, 2023) advocates for the use of the aSSKINg framework as part of an individualised plan of preventative care. Evidence-informed recommendations and a standardised clinical pathway are currently under development for the reduction of pressure ulcers and their associated harms. However, there is an urgent need to include skin tone assessment in the skin assessment aspect of the aSSKINg framework.
Challenges of implementing prevention strategies for people with dark skin tones
Major barriers to the implementation of pressure ulcer prevention strategies have been identified, including heavy workload, inadequate staffing levels, shortage of resources/equipment, insufficient training and non-inclusive assessment tools (Etafa et al, 2018). Limited access to up-to-date and evidence-based literature, in addition to a lack of multidisciplinary working, have also been identified as barriers to the development of prevention programmes. Certain beliefs and practices may also influence the willingness of patients with dark skin to discuss their symptoms or report discomfort (Dhoonmoon et al, 2023). This can further hinder early intervention and treatment of pressure ulcers.
Key enablers to implementation of evidence-based practice have been identified, including high levels of self-reported knowledge and skills in relation to pressure ulcers, responsive community equipment provision where damage is recognised early and integrated team working (Taylor et al, 2021). However, these enablers have been proposed in relation to people with light skin tones only. Therefore, it is evident that there is a need to focus on upskilling clinicians and providing a supportive training environment, to address their concerns about skin inspection and detection of the early stages of damage – especially in people with dark skin tones – and difficulties in initiating conversations with patients about risk and behaviour change [Box 4].
Conclusion
While pressure ulcers are preventable in most cases, they pose a substantial economic, health-related and social burden, and can significantly diminish patients’ quality of life (Demarré et al, 2015; Mervis and Phillips, 2019). There is a need for improved healthcare practices and practitioners who can deliver equitable care in order to address the unique challenges faced by patients with dark skin tones. Increasing awareness of the different manifestations of pressure ulcers in dark skin and improving education requires a comprehensive and multidisciplinary effort. However, by receiving training that encompasses diverse skin tones, all members of the clinical team will be able to fill the gaps in their knowledge and deliver more effective, quality care to patients with pressure ulcers.