1 Bullous pemphigoid is blistering between the epidermis and dermis.
Bullous pemphigoid is an autoimmune disease in which antibodies are formed against collagen in the hemidesmosomes of the basement membrane. The response is both inflammatory and immune, with release of cytokines from the T- cells leading to complement activation, recruitment of neutrophils (acute inflammatory cells) and the release of proteolytic enzymes.
Bullous pemphigoid initially begins as a rash and progresses to bullae in weeks to months, typically presenting in the axillae, on the flexor surface of the forearms, medial thighs, trunk, and abdomen [Figure 1]. It most commonly affects patients between the ages of 60 and 80, but can also be seen in children.
2 Scleroderma is a rare autoimmune disease that leads to hardening of the skin.
Scleroderma is a chronic systemic disease of progressive inflammation and tissue fibrosis and includes occlusion of small blood vessels. This presents as skin tightening, discolouration, itching and Raynaud’s phenomenon. The latter is a constriction of small blood vessels of the hands, resulting in painful, cold and bluish fingers [Figure 2]. Scleroderma can also cause difficulty eating, heartburn, constipation that alternates with diarrhoea, a dry cough, joint pain and muscle weakness
3 Epidermolysis bullosa presents as fragile skin that blisters easily.
Epidermolysis bullosa is a rare, inherited condition, which is due to structural defects in the dermo-epidermal junction. Trivial mechanical trauma and shear stress can provoke skin blistering, erosion, and ulceration. Epidermolysis bullosa simplex presents with blistering, pruritus, pain, nail abnormalities, dyspigmentation, keratoderma, erosions, and scarring. Repeated chronic insult to the epidermis is thought to predispose patients to a mildly elevated incidence of skin cancers [Figure 3].
4 Sickle cell disease can lead to leg ulcerations.
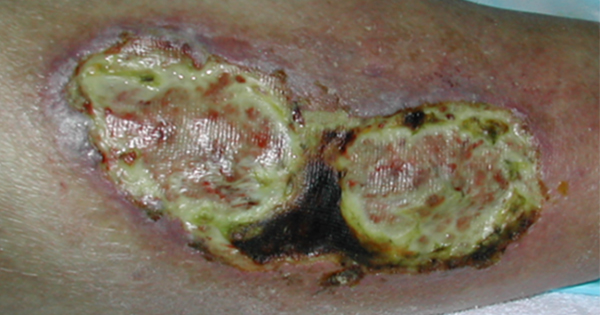
Sickle cell disease is an inherited form of anaemia due to abnormally crescent-shaped red blood cells that cannot deliver enough oxygen to the cells. The triggering event for sickling is often hypoxaemia that deoxygenates the sickle haemoglobin and makes it a rigid sickle shape. The sickled red blood cell occludes the blood vessels, causing severe painful ischaemic attacks in the affected areas or organs. Leg ulcers are a chronic painful problem [Figure 4]. The most common sites are the medial and lateral malleoli. Healing is delayed and infection may occur.
5 Pyoderma gangrenosum has a unique presentation – think the letter P.
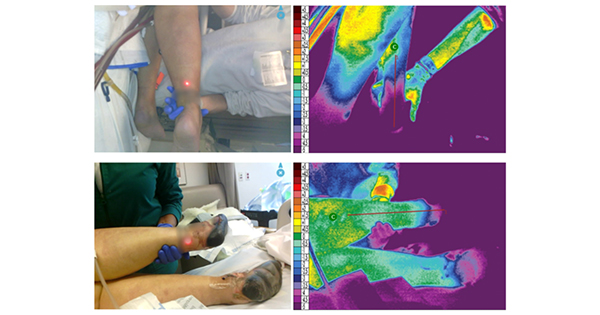
Pyoderma gangrenosum is a rare inflammatory condition of skin presenting as a pretibial (or peristomal) wound. It is progressive, with pain beyond expected, purple wound edges and pathergy. Pyoderma gangrenosum is a genetic mutation leading to a profound dysregulation of both the innate and adaptive immune systems. It is not caused by infection or gangrene.
Pyoderma often occurs as a secondary complication of any skin cut or trauma [Figure 5]. One of the most important features of the disease is pathergy. Pathergy is defined as an exaggerated response to a minor skin injury, or worsening of an existing wound with minimal insult or trauma. This untoward response has significance for the provider because debridement and simple wound care are likely to make the wound worse.
Pyoderma gangrenosum is associated with several systemic diseases including inflammatory bowel disease, rheumatoid arthritis and other autoimmune and inflammatory conditions. Pyoderma gangrenosum should not be confused with pyogenic granuloma, a separate entity, but with an equally ill-fitting name.
6 Cutaneous vasculitis often presents as petechia.
Vasculitis is a group of autoimmune diseases that lead to inflammation of blood vessels. This disease could be called ‘capillaritis’, which presents as progressive and pruritic purpura (petechiae). Vasculitis can be systemic or localised; therefore, presentation varies from mild redness and irritation to occlusion of blood vessels and ischaemia of the affected area [Figure 6].
7 Marjolin’s ulcers are cancers that can develop in burn scars, often years after the initial injury.
One of the most common types of skin cancer associated with burns is squamous cell carcinoma. This type of cancer typically appears decades after the initial burn injury and is known as Marjolin’s ulcer. These tumours form due to chronic inflammation, repeated injury and impaired immune surveillance. Scars from other wounds that heal by secondary intention are also at risk. Marjolin’s ulcer usually does not look like a skin cancer; instead, it appears as a nonhealing wound in the scar.
Most Marjolin’s ulcers are squamous cell carcinoma, although basal cell carcinoma and melanoma have been infrequently reported. It is important to biopsy these lesions because they become metastatic quickly [Figure 7].
8 Calciphylaxis appears in patients with end-stage kidney disease.
The lesions initially appear as indurated plaques and nodules, livedo or purpura. They will manifest in groups, bilaterally, and have a short timeframe of progression to stellate, malodourous ulcers with black eschars [Figure 8].
An overwhelming proportion of these patients require opiate-based painkillers to manage the pain. The biochemical conditions – including hyperphosphataemia, hypercalcaemia, and hyperglycaemia – help incite the transformation of vascular smooth muscle cells into osteoblast-like cells, thereby establishing the mechanics for vascular calcification by ectopic bone formation within the vessel walls (Nigwekar et al, 2018).
9 Factitious dermatitis or dermatitis artefacta is often a diagnosis of exclusion.
This type of skin injury is from the deliberate creation of wounds on skin, hair, nails, or mucosa, often to meet complex psychological needs. This condition is caused by multiple genetic and psychological factors. It presents with multiple superficial, self-inflicted skin lesions of variable shape, size and depth on accessible areas like the face, arms and abdomen. Patients will often deny inflicting these wounds.
The typical presentation includes cutaneous lesions, which are bizarre and mimic many of the known inflammatory reactions in the skin. The lesions may be circular blisters or erosions, burns, cryodamage, excoriations, urticarial lesions, haemorrhages, indurations or necrosis. The fabricated history that follows is usually ‘hollow’, and there is no complete description of the genesis of individual skin lesions that appear suddenly and fully formed on accessible sites. Usually, the patient has a history of chronic skin conditions and personal or familial history of psychiatric conditions. [Figure 9].
10 Brown recluse spider bites evolve rapidly.
Brown recluse spiders (Loxosceles reclusa) and other species in the genus Loxosceles have a toxic venom that contains the dermonecrotic agent sphingomyelinase D. In one study of clinically diagnosed brown recluse bites, skin necrosis occurred 37% of the time, while systemic illness occurred 14% of the time (Wright et al, 1997).
Initially the spider bite may go unnoticed, as it is not painful, but over the next 6 to 8 hours it can progress to severe pain, itchiness, and a clear fluid-filled cyst with a red surrounding border [Figure 10]. Because of the frequency of naming many wounds recluse spider bites, a mnemonic was developed to show contrary criteria to spider bites [Box 1; Stoecker et al, 2017].