Surgical wound complications such as surgical site infection (SSI) and surgical wound dehiscence (SWD) represent a considerable issue in global healthcare across surgical disciplines (Sandy-Hodgetts et al, 2022a). A panel meeting of clinical experts was convened to examine post-incisional care and dressing selection in OB-GYN practice. The attending clinicians work across the APAC region, united by a passion for wound care and improving patient outcomes.
The findings of this panel meeting follow on from previous work across geographical regions and clinical disciplines [Box 1], and had the following aims for topics of discussion:
- Dressing selection and protocol in surgical wounds
- Dressing wear time
- APAC region-specific considerations, and specific considerations for OB-GYN practice
- Properties of the ‘ideal dressing’.
The importance of post-operative wound care
The panel agreed that, from the patient’s perspective, the quality of the skin incision is very important; from the initial incision through to wound closure, it is an essential aspect of post-operative care. Good quality healing with minimal scarring is also particularly important to many patients. To achieve this, it was recommended that surgeon involvement should be an active role from the creation of the incision to decision making regarding post-operative care of the patient.
The ability to take an active role begins very early in a healthcare professional’s career through the embedding of wound healing and skin integrity education within medical and nursing undergraduate curriculum.
Surgical wound management differs across the APAC region, being either surgeon- or nurse-led, or a combination of both. In Australia, particularly in the public healthcare system, this practice is predominantly nurse driven. Although there are differences, it is important to use evidence-based practice, regardless of the discipline.
Undisturbed wound healing
While post-operative dressing protocols vary according to geographical region and individual healthcare institutions, recent evidence has shown the benefits of undisturbed wound healing (UWH; Brindle and Farmer, 2019).
UWH is where a dressing is left in situ for as long as possible (when clinically indicated) to minimise wound disturbance and facilitate wound healing. The reduced frequency of dressing changes may also prevent an increase of medical waste and inefficient use of dressings. Specific clinical indicators for change may include leakage or saturation, or signs of infection, and are at the clinical judgement of the attending healthcare professional in adherence to local policies and guidelines.
Dressing selection and protocol
In clinical practice, clinicians may be moving towards UWH, and then using advanced dressings to prevent scar formation (Monstrey et al, 2014; Rousseau et al 2022). Advanced dressings may include combinations such as hydropolymers, hydrocolloids and silicone, while conventional dressings include gauze and tape (Freedman et al, 2023). The panel reflected on the availability of different types of dressings and that their accessibility may be dependent upon the healthcare setting (e.g. government-run or private).
Some of the panel members discussed specific considerations for dressing selection in OB-GYN. These considerations include the moisture vapour transmission rate or ‘breathability’ of dressings to be used in caesarean section (c-section) incisions and breast abscesses, as well as the ability of the patient to shower while keeping their wound dry.
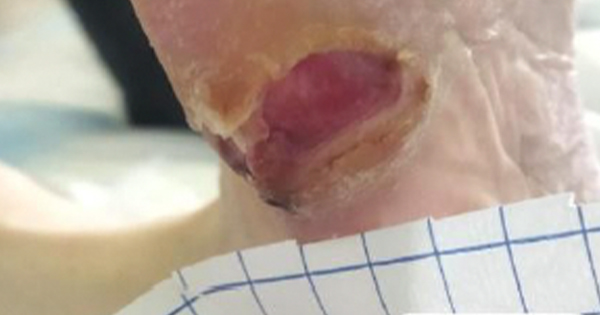
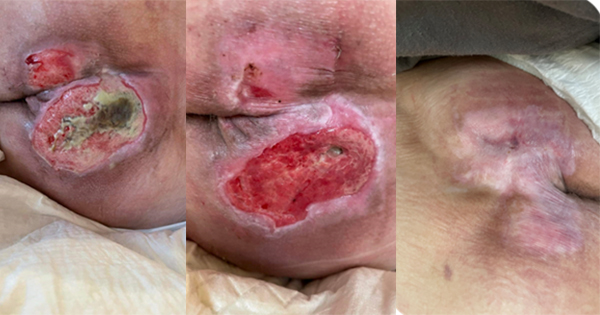
Wound healing may also be impacted by the number of c-sections a mother has undergone (Dodd and Crowther, 2007). Wound-related complications, such as wound discharge or dehiscence, delay healing and result in significant morbidity and mortality (Sandy-Hodgetts et al, 2022a). Since post-operative incision wound care impacts upon patient well-being and outcomes, early detection of wound complications is crucial and may prevent hospital readmission (Pinto et al, 2016, Nasab et al, 2018).
The expert panel emphasised the importance of post-operative evaluation of the wound. Conditions that can impact upon wound healing (e.g. obesity, immunocompromised state, or diabetes) should be taken into account, along with the choice of suture (Alma et al, 2023; Bootun, 2013; Leth et al, 2011; Spampinato et al, 2020; Zucker et al, 2019).
It was discussed that, in countries with a hot and humid climate, there may be an increased risk of SSI (Sahtoe et al, 2021). In Thailand, for example, medical adhesive-related skin injuries (MARSI) can be problematic in 10–20% of patients, which may affect wound healing (Upton et al, 2019). Therefore, it was recommended that dressing selection should consider the ease of removal to prevent injury on dressing change.
Current challenges in practice in incision care management
The challenges faced are unique to each surgeon and country in the APAC region. However, the panel discussed some common areas in which challenges arise.
Hand hygiene
Proper hand hygiene decreases the proliferation of microorganisms, thereby reducing infection risk, overall healthcare costs, and length of hospital stay (Toney-Butler et al, 2023). Hand hygiene is one of the single most important practices for reducing the risk of infection transmission in the healthcare setting. However, at times, it is not adequately recognised among healthcare professionals and compliance remains low in some areas (Toney-Butler et al, 2023).
Patient and clinician education
Effective patient education has the potential to reduce healthcare expenditure and prevent serious complications (Callender et al, 2021). An increase in patient education would be valued, particularly about when and how often dressing changes should be undertaken following surgery. It was generally agreed that patients should be sent home with relevant information written in lay terms on how to care for their wound and when to seek medical assistance.
It was noted during the meeting that healthcare professionals should receive regular education to update practice and to ensure that advanced technologies are used appropriately (Atkin, 2020). The expert panel particularly recommended educating doctors about the risk of infection and newer wound dressings on the market.
The patient voice
Engagement of patients and their carers and the development of therapeutic relationships are key to understanding post-operative care needs in the home setting. Providing education on home care improves health literacy and can improve healing outcomes. At times, the absence of patient compliance is associated with poor healing outcomes, impaired quality of life and frustration for both patients and clinicians (Gallagher, 2022). The expert panel discussed some examples of the importance of patient engagement and how this can improve outcomes. Key factors to improve patient engagement are shown in Box 2.
Workload issues
The three main drivers which determine the level of workload resource in wound care are: the time it takes to heal a wound, the frequency of dressing changes and the incidence of complications such as wound infection (Lindholm and Searle, 2016). Reducing healing time and dressing change frequency as well as preventing wound complications may free up resource and reduce workloads (Lindholm and Searle, 2016).
Scar formation
Scarring as a result of surgical procedures is a cause of concern for patients (O’Reilly et al, 2021). Scar formation following a c-section has the potential to affect a woman’s wellbeing and impact her perception of cosmesis (Gaertner et al, 2008). The choice of wound dressing is important as it may influence post-operative surgical wound healing and scar formation (Son and Harijan, 2014).
Properties of the ideal dressing in OB-GYN patients
The expert panel agreed that it is challenging to create the ideal dressing for OB-GYN patients, but there are key properties that would be expected as a minimum in the APAC region for the OB-GYN population. The panel agreed that the points listed in Table 1 should be considered as the essential properties for an ideal dressing.
The expert panel acknowledged that there is no ‘one size fits all’ ideal dressing, but rather the type of dressing is impacted by type of surgery, skin tone and individual patient need. In addition to those listed in Table 1, the panel recommended several additional properties which should be incorporated into wound dressings for specific patients. For example, wound infection is more common in countries with a hot/humid climate (Sahtoe et al, 2021) and in the obese patient (Al-Kharabsheh et al, 2021). The inclusion of an antibacterial element in the dressing (e.g. silver alginate base or an antibiotic embedded mesh) may be suitable for some patients. Finally, the panel recommended that dressings that do not leak, are hypoallergenic and which can remain in situ for up to 7 to 10 days would be ideal.
Role of enhanced recovery after surgery (ERAS)
ERAS programmes reduce morbidity in terms of providing effective pain control, reducing length of stay, and facilitating an earlier return to normal activities (Gupta et al, 2022). They represent a significant shift in peri-operative care through the replacement of traditional practices with evidence-based practices as necessary, covering each phase of the surgical process (i.e., pre-operative, intra-operative and post-operative care; Altman et al, 2019; Achrekar, 2022; Li et al, 2023). The panel observed that for ERAS to work effectively, the programme requires a multidisciplinary approach with all stakeholders engaged and the appropriate infrastructure and resources provided by the healthcare facility.
The selection of wound dressings plays a crucial role in ERAS. Silicone-based dressing adhere easily to dry skin but do not stick to the fragile tissue surrounding the wound, potentially alleviating pain associated with post-operative mobilisation (Silverstein et al, 2011). As these dressings can be applied and removed without damaging the surrounding epidermis, they are expected to minimise the psychological stress experienced by patients (Zillmer et al, 2006; Woo et al, 2009). Furthermore, the antimicrobial effects of silver-containing products may also contribute to pain mitigation (Davies et al, 2017).
Nutrition also plays a vital role in ERAS protocols. Maintaining appropriate nutritional status post-operatively has been shown to reduce the length of hospital stays and rates of post-surgical complications such as delayed wound healing, anastomotic leaks, or pulmonary complications (Nelson et al, 2019). In their guidelines, the ERAS Society recommends a regular diet within the first 24 hours after gynaecological surgery, with high-protein diets recommended for consideration in the post-operative management of surgical patients (Nelson et al, 2019).
Conclusions
Post-incisional care can vary significantly according to factors such as geographical region, healthcare system and individual patient considerations. While it was agreed that there is no ‘one size fits all’ dressing solution, the panel discussed the key properties of the ‘ideal’ dressing and post-surgical wound treatment protocol. The panel also agreed on the importance of UWH.