The management of surgical incisions is a critical component of perioperative infection control and wound healing, supporting optimal patient recovery. This is particularly relevant in orthopaedic and joint surgery where unique incision sites, procedural complexity and variability in patient baseline conditions demand more rigorous dressing selection and management strategies. Additionally, the use of metal implants and the challenges associated with managing implant-related infections make it essential to minimize wound healing complications. With the growing adoption of Enhanced Recovery After Surgery (ERAS) protocols, evidence-based and standardized incision care has emerged as a key pathway for enhancing surgical quality (Wounds UK, 2020; Morgan-Jones et al, 2021; Sandy-Hodgetts et al, 2022).
To advance the standardization and evidence-based practice of postoperative incision care among orthopedic surgeons in China, a dedicated consensus meeting was held in Nanjing, China, building on the work of other international surgical panels [Box 1].
The summit brought together orthopedic experts in arthroplasty, trauma and spine surgery from 12 leading tertiary hospitals across China. Discussions focused on key issues in postoperative incision care, including clinical challenges, the prevention and management of complications, and the selection and ideal properties of dressings, culminating in a consensus that reflects the clinical realities in China. Comprehensive surgical incision care spans the entire perioperative period, encompassing preoperative risk assessment and optimization, standardized intraoperative techniques and continuous postoperative monitoring and intervention (Morgan-Jones et al, 2021). Effective surgical incision care can significantly reduce infection rates, enhance the quality of healing, shorten hospital stays and align with the cost-containment objectives of China’s current Diagnosis-Related Group (DRG) and Diagnosis-Intervention Packet (DIP) payment systems.
Appropriate incision care and dressing selection can promote optimal wound healing and significantly reduce incision-related complications, particularly surgical site infections (SSIs). These improvements contribute to accelerated patient recovery, shorten the length of hospital stay, reduce healthcare costs and ultimately enhanced patients’ safety and overall quality of care.
Current landscape of postoperative incision management in China
Postoperative incision care refers to a series of perioperative assessments and symptomatic monitoring of the patient, with the aim of promoting wound healing, preventing infection and minimizing incision-related complications. China’s vast geographic diversity and uneven distribution of healthcare resources present unique challenges in standardizing postoperative incision care across different regions and healthcare tiers. The expert panel agreed that promoting access to high-quality medical resources and standardizing dressing management strategies nationwide are crucial for improving patient outcomes and healthcare efficiency. Evidence-based incision care and appropriate dressing selection can reduce the risk of surgical site infection, accelerate recovery, shorten the length of hospital stay, reduce medical costs, and further strengthen patient safety and quality of care.
Challenges and strategies for access to high-quality medical resources
Despite China’s vast geographic and demographic scale, access to medical resources remains uneven due to significant regional disparities. Currently, the advanced medical resources are concentrated in major metropolitan areas such as Beijing, Shanghai, Guangzhou and the provincial capitals of the southeastern coastal region in China. In contrast, medical capabilities in primary healthcare facilities in western regions are relatively weak. Through initiatives such as medical alliances, integrated hospital networks and specialty consortia, advanced medical standards and techniques are being progressively extended to underserved regions. These efforts provide an important foundation for standardized and consistent postoperative incision care.
Opportunities arising from healthcare payment reform
With the ongoing reform of healthcare payment systems, including the implementation of DRG/DIP models, greater attention is being paid to the use of high-quality, cost-effective medical consumables in postoperative care. China’s national volume-based procurement policy for high-value medical supplies has further reduced pricing barriers, making high-performance dressings with demonstrate a clinical and economic benefits more accessible to a broader patient population.
Impact of regional and climatic variations on dressing requirements
The hot and humid climate in southern China requires dressings with superior breathability and water resistance to prevent moisture accumulation and maintain an optimal healing environment. In contrast, western and northeastern regions where medical facilities are sparse and patient follow-up is often challenging require dressings that offer longer wear times and greater stability to minimize the frequency of dressing. Therefore, selecting dressings that can accommodate these diverse regional characteristics is essential for ensuring broad clinical applicability. Challenges related to limited access to medical resources, particularly in remote areas, can be mitigated through the standardization of incision care practices and wider dissemination of high quality medical products, supported by healthcare consortia and integrated medical networks (Su et al, 2022).
Factors influencing postoperative incision healing
The expert panel emphasized that proper incision healing is critical to reduce the risk of surgical site infection, and to improve the pace of recovery and overall treatment outcomes.In the context of ERAS implementation and ongoing healthcare payment reform in China, the identification and optimization of risk factors affecting wound healing have become major clinical priorities. Incision healing is influenced by numerous factors, which can be broadly categorised as patient-related and medical-related factors.
Patient-related factors
- Underlying diseases and metabolic state: Conditions such as diabetes, chronic kidney disease and hypoproteinemia can impair tissue oxygen delivery, disrupt normal wound-repair processes, and weaken immune function, leading to delayed healing and an increased risk of surgical site infection (Hom and Davis, 2023; Sangha et al, 2024)
- Age and lifestyle: Advanced age, smoking and obesity are associated with reduced skin tolerance, impaired microcirculation, and a diminished immune response
- Skin integrity and medical history: Patients with a history of keloid formation, long-term corticosteroid use, or prior radiotherapy at the surgical site require special consideration due to compromised healing capacity
For patients with one or more high-risk factors, such as advanced age, smoking, obesity, diabetes, malnutrition, autoimmune disorders (e.g. rheumatoid arthritis, systemic lupus erythematosus) or long-term immunosuppressive therapy, the use of antimicrobial dressings (e.g. silver-containing dressings) are recommended. These dressings help reduce the risk of surgical site infection and support wound healing by maintaining a moist environment, managing exudate and preventing microbial colonisation. They are particularly suitable for the management of postoperative incisions at high risk of infection (Mundi et al, 2023; Srivastava et al, 2025).
Medical-related factors
- Site of incision and surgical procedure: For instance, an anterior knee incision following a total knee arthroplasty (TKA) is at a higher risk for blister formation due to high skin tension and frequent joint movement (Lyons et al, 2022)
- Implant-related risks: The presence of a metal implant or prosthesis substantially increases the complexity and cost of treatment if an infection occurs (Cao et al, 2024)
- Postoperative management strategy: Inappropriate dressing selection or excessively frequent dressing changes may disrupt the delicate microenvironment of the wound, thereby delaying the healing process (Pickles et al, 2022; Sun et al, 2023)
- Other factors: Radiation exposure, insufficient psychological support and inadequate patient education regarding postoperative precautions.
Recommendations for managing incisional complications
Incisional complications are broadly classified as either infectious or non-infectious. Both can compromise patient comfort and recovery, potentially leading to extended hospital stays, increased risk of infection and higher overall healthcare costs (Wounds UK, 2020; Rosa et al, 2023).
Responsibilities in monitoring and evaluating incision healing
- Normal healing process: Recognition of the expected wound healing stages
- Monitoring of incision healing process should include:
- Assessing the healing process
- Tracking systemic responses
- Evaluating functional recovery
- Evaluation of incision healing: Structured assessment against clinical criteria
- Standard of incision healing: Applying defined benchmarks to determine progress and outcomes.
Infectious complications
Common types of infectious complications include:
- Superficial surgical site infection (SSI): Typically develops three to seven days after surgery and presents with redness, swelling, warmth, pain and exudate (Gajda et al, 2023; Lin et al, 2024)
- Deep infection: Often associated with prosthetic implants and more complex to treat, frequently requiring surgical intervention together with antimicrobial therapy (Cao et al, 2024).
Recommendations
Preoperative phase:
- Optimize the patient’s medical condition through the management of comorbidities (e.g. strict glycemic control in diabetes) and enhancement of nutritional status (Tarabichi and Parvizi, 2023)
- Conduct screening for colonization of resistant bacteria (e.g. MRSA) when appropriate and implement targeted preoperative decolonization protocols (Tarabichi and Parvizi, 2023; Clarke et al, 2025).
Postoperative phase:
- Strictly aseptic procedures during dressing change for incision and closely monitor the signs of infection (redness, swelling, warmth, pain). Microbial cultures should be ordered when necessary (Wounds UK, 2020; Rosa et al, 2023; Sun et al, 2023)
- To maintain a stable microenvironment, excessively frequent or unnecessary dressing changes should be avoided
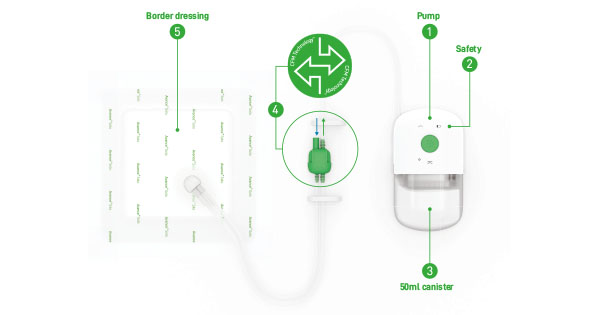
- Based on a thorough risk assessment, consider advanced therapies such as negative pressure wound therapy or topical antimicrobial agents for high risk patients(Ainslie-Garcia et al, 2024; Srivastava et al, 2025).
- For patients at high risk of postoperative infection, such as those with diabetes, immunosuppression, malnutrition or prosthetic implants, postoperative dressings with antimicrobial properties, such as silver-containing dressings, are recommended. These dressings help reduce risk of SSI by preventing pathogen colonization, managing exudate and maintaining a moist healing environment, particularly during the critical early postoperative phase.
Non-infectious complications
1. Tension blisters
Tension blisters are defined as the formation of fluid-filled sacs under the epidermis. These are most common over high-tension areas, such as the anterior knee. Key contributing factors include premature mobilization, poor dressing conformability (for example, at the edge of traditional nonelastic dressings) and high local shear forces (Cole et al, 2020; Anusitviwat and Yuenyongviwat, 2025).
Recommendation: Select highly conformable, hypoallergenic dressings (e.g. those with a soft silicone adhesive). Avoid tight dressings on the wound and premature or excessive activity.
2. Incisional dehiscence and delayed healing
Incisional dehiscence is the separation of the edges of a closed surgical skin incision, which may or may not be accompanied by the exposure or protrusion of subcutaneous tissues, organs or implants. It may occur in one or more places, involve the entire length of the incision, affect some or all of the tissue layers and it may or may not be accompanied by infection. These can be linked to malnutrition, ruptured blisters, poor wound closure technique, localized infection or premature weight-bearing (Hom and Davis, 2023; Sangha et al, 2024).
Recommendation: Reinforce perioperative nutritional support, minimize tension on the incision closure and avoid frequent dressing changes until the wound is stable.
3. Skin tears and medical adhesive-related skin injury (MARSI)
These are prevalent among patients of advanced age, those with fragile skin or those undergoing frequent dressing changes with highly adhesive materials (Cole et al, 2020; Yang et al, 2025).
Recommendation: Utilize hypoallergenic dressings with gentle adhesion (e.g. soft silicone). Reduce the frequency of dressing changes and follow proper removal techniques to minimize skin trauma.
4. Other dermatological reactions
This category includes conditions such as proliferative scarring, skin allergies, neurodermatitis and subcutaneous neuroma.
Recommendation: Thoroughly review the patient’s allergy history and use products with demonstrated skin compatibility. Should a reaction occur, it must be addressed promptly.
The importance of the undisturbed wound healing (UWH) philosophy
The expert panel unanimously emphasised the importance of minimizing external disruption to the healing process. They endorsed the philosophy of UWH to optimize the wound environment and enhance the quality of healing (Sandy-Hodgetts et al, 2022).
To implement this approach effectively, the following management strategies are recommended:
- Recommendation 1: Extend dressing wear time. Use dressings designed for wear of five days or longer, unless contraindicated. This practice reduces the mechanical disruption and risk of contamination associated with frequent changes (Morgan-Jones et al, 2021)
- Recommendation 2: Avoid unnecessary dressing changes. Routine dressing changes performed merely for “observation” or out of habit are discouraged
- Recommendation 3: Establish clear indications for dressing changes. A dressing should only be changed under the following specific circumstances:
- The dressing becomes saturated with exudate or begins to leak
- Wound protection is compromised due to rolled edges or disruption of the dressing
- Presence of clinical signs of infection at the incision site (e.g. redness, swelling, warmth or pain)
- The patient develops an adverse reaction, such as skin irritation or an allergic response to the dressing.
Key characteristics of an ideal postoperative dressing
The expert panel concluded that an ideal postoperative dressing must extend beyond the basic functions of exudate management and protection. It should offer multiple advantages in promoting healing, preventing infection, reducing complications and improving patient experience. The comprehensive performance of a dressing is particularly vital in the context of China’s vast geography, the high demand for home-based wound care and the uneven distribution of medical resources. Based on clinical experience and evidence-based research, the consensus is that an ideal dressing for orthopedic postoperative incisions should exhibit the following core characteristics (Mundi et al, 2023; Sun et al, 2023; Srivastava et al, 2025)
1. Wound healing promotion
The dressing should maintain an optimal moist environment and minimize disturbances from frequent changes to support UWH. Advanced dressings may enhance healing by providing antimicrobial protection or improving the wound microenvironment through specialized design features (Sun et al, 2023).
2. Effective exudate management
The dressing must effectively absorb and lock away exudate to prevent maceration of the wound bed and surrounding skin. This capability reduces the frequency of dressing changes and is suitable for incisions with moderate to high levels of exudate (Mundi et al, 2023).
3. Antimicrobial and barrier protection
The dressing should provide a reliable bacterial barrier and ideally possess antimicrobial or bacteriostatic properties to protect the incision during the vulnerable postoperative period.
Silver-containing dressings are recommended for high-risk incisions, such as those involving implants, immunocompromised patients
or contaminated surgical sites. The broad- spectrum antimicrobial activity and sustained barrier function make them an effective option for reducing the risk of SSIs (Ainslie-Garcia et al, 2024; Anusitviwat and Yuenyongviwat, 2025; Srivastava et al, 2025).
4. Superior conformability and flexibility
The dressing must conform seamlessly to body contours, especially over mobile areas like joints. This reduces shear and friction forces, thereby minimising the risk of complications like tension blisters and skin tears (Cole et al, 2020).
5. Hypoallergenic and safe
The dressing should be made from low-irritant materials, such as a soft silicone adhesive, to decrease the risk of Medical Adhesive-Related Skin Injury (MARSI). This is especially important for older patients and individuals with fragile skin (Yang et al, 2025).
6. Facilitates clinical observation
The dressing should allow clear assessment of the peri-incision skin and the extent of wound exudate.
7. Waterproof yet breathable
The dressing should provide an effective waterproof barrier while maintaining a high Moisture Vapour Transmission Rate (MVTR), making it particularly suitable for humid climates in southern China and for patients who need to shower after surgery (Su et al, 2022).
8. Patient comfort
The dressing should be lightweight, soft, flexible and adaptive to the patient’s mobility after surgery. This reduces discomfort and the sensation of a foreign object, thereby improving patient compliance and adherence to treatment.
9. Suitable for at-home care
The dressing should be easy to apply, offer long-lasting adhesion and not require frequent
changes. This facilitates self-monitoring and care for patients at home or those undergoing remote follow-up consultations.
10. Reduced scar formation
The dressing can lessen tension on the incision, maintain skin smoothness and lower the risk of keloid scar development. This makes it particularly suitable for patients who desire better cosmetic outcomes for their incisions following joint surgery. Experts advise that the selection of a postoperative dressing should be based on the specific surgical procedure, the individual patient’s risk factors and their desire for at-home care. The primary objectives are to minimise disturbance to the wound, promote a moist healing environment and lower the risk of complications. This approach supports ERAS protocols and facilitates high-quality clinical practice in postoperative management.
Future outlook and summary
There remains a significant opportunity to improve the standardization of postoperative incision care in China. Drawing from the discussions at this conference, the orthopedics experts have proposed the following recommendations for future development:
Establish a tiered protocol for postoperative incision care
- Encourage more clinical research and real-world evidence (Ainslie-Garcia et al, 2024; Srivastava et al, 2025)
- Accelerate the development of specialized dressings tailored to the unique requirements of orthopedics procedures (Lei et al, 2024; Anusitviwat and Yuenyongviwat, 2025
- Enhance the education and training for healthcare professionals on evidence-based dressing selection and risk assessment.
By consolidating the clinical experience of representative orthopedics experts from China, this conference has established a consensus on recommendations for postoperative incision care. The aspiration is that this consensus will lay a foundation for actionable clinical pathways and practical standards. The nationwide implementation of these standards will help enhance the quality of postoperative recovery for patients and improve the overall efficiency of the nation’s healthcare system.