It has been established that post-surgical incision care is a vital part of the patient journey and must be optimised, particularly in terms of reducing the risk of infection and associated complications (Sandy-Hodgetts et al, 2017; 2018; Morgan-Jones et al, 2020). With this in mind the objectives of the meeting were:
- To clarify global views on incision care and dressing selection in surgical wounds
- To discuss key areas and reach consensus on recommendations
- To discuss and agree on the 6 properties of the ‘ideal’ dressing in managing post-surgical incisions (Morgan-Jones et al, 2020).
The importance of dressing selection in surgical wounds
Dressing selection plays a key role in post-surgical incision care (WUWHS, 2016). However, there is considerable discourse regarding the efficacy of wound dressings for prevention of surgical site infection (SSI), a potential complication following any type of surgery (Dumville et al, 2016; Sandy-Hodgetts, 2017). Protection of the incision site is of key importance, particularly with regard to managing the risk of SSI and surgical wound dehiscence (SWD). More importantly, for improved patient wellbeing and outcomes, is the ability to create an optimal wound healing environment. With the advent of the antimicrobial resistance age, post-operative incision management requires extensive consideration, with reports of global prevalence of SSI ranging from 2–15% depending on multiple factors, including the type of operation (ECDC, 2018). Some reports suggest that SSIs affect up to one-third of patients who have undergone a surgical procedure, and is one of the leading casues for hospital readmission, with 3% of patients dying from an SSI (Minski, 2019).
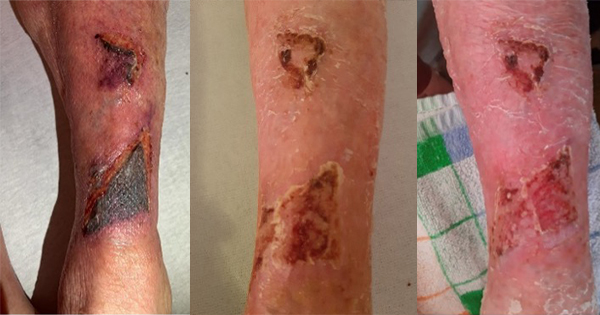
It is also important to note that SSI is only one type of post-surgical complication: not all complication is related to infection (Sandy-Hodgetts et al, 2020). Surgical wound complication as a broad term can also include, but is not limited to (Sandy-Hodgetts et al, 2020):
- SWD
- Hypergranulation
- Peri-wound maceration
- Scarring
- Medical adhesive-related skin injury (MARSI).
Dressing wear time
It was agreed that it is important to choose a dressing that can manage exudate and afford extended wear time wherever possible. The concept of undisturbed wound healing (UWH) is of particular importance in surgical wounds, as using a dressing with an increased wear time and keeping the dressing in situ can help to reduce the risk of contamination (Morgan-Jones et al, 2020). It was agreed that while UWH may be of benefit in surgical wounds, more evidence is needed in order to inform care guidelines.
While exact protocol varies across geographical areas and according to individual patient needs, it was agreed that, in general, the wound should be left undisturbed for as long as possible after surgery. Simply, ‘leave the skin and wound alone’ was broadly agreed as the optimum way to encourage healing in wounds where UWH is possible. There are exceptions to this and it was agreed that the dressing should be changed if there is a clear clinical reason to do so. Leaking or saturation are agreed to be clear reasons to change the dressing. Monitoring the dressing for signs of infection is also a consideration, although it should be noted that, in the first days after surgery, any inflammation observed is likely to be due to normal wound healing processes and is unlikely to be due to infection, which is not normally visible until day 3 or 4 post-surgery. Therefore, managing the wound is the key concern (Sandy-Hodgetts et al, 2013; 2017; 2019). There is a need for awareness around UWH in surgical wounds. Education about normal wound healing processes and what to look out for as surgical wounds heal may help to guide appropriate patient selection and allow wider use of UWH. Potential indicators that dressing change is necessary (or preferred) include:
- Saturated dressing
- Dressing leakage
- Geographical factors – in some areas, patients have to travel long distances and may have limited resources available at home, so prefer their dressing to be changed before discharge
- Staffing/competency issues – who carries out the dressing change can influence decision-making, depending on the structure and staff being in place to safely change the dressing
- Social influences and patient preference – the patient may prefer the dressing to be changed.
APAC region-specific considerations
There are some region-specific considerations in dressing selection and wound healing, including factors around the dressing or cultural considerations. For example, in some humid/tropical climates, waterproof dressings are very important. Patients travelling long distances can also be an issue in dressing selection and change frequency; it is important that patients can be confident they have the information and resources they need when they are far from the hospital.
Patient optimisation prior and after surgery utilising the Enhanced Recovery After Surgery (ERAS) protocols is used in some areas, which include post-surgery dressing requirements (ERAS Society, 2016). While it is not universally embedded in clinical practice, early adopters have seen improved outcomes (Gustafsson et al, 2013; Kaye et al, 2019). It was agreed that good pre-operative assessment can generally improve outcomes. The WHO surgical checklist (WHO, 2020) is also used in some settings; it was agreed that using checklists and ensuring that a specific staff member takes responsibility for checklists, and that senior staff are vigilant in standard-setting, can have a positive effect.
It is also important to note that product availability acorss differing geographic regions can present issues for dressing choices in clinical management, as not all dressings are widely available in all care settings. Cost is also a consideration. However, in selecting an appropriate dressing, the total costs of care should be considered in tandem with the individual dressing or unit price. Total cost represents more than the unit cost and can be reduced if the dressing is effective and can stay in place for longer, providing greater value with reduced length of stay and frequency of dressing changes.
Patient-related factors
It was agreed that patient comfort is very important. It is vital that the patient is provided with information on all aspects of their treatment and trusts the clinician. In terms of comfort, a dressing that is easy to remove without pain or irritation is needed. MARSI is a potential issue, particularly blistering around the wound (McNichol et al, 2013; Fumarola et al, 2020). Using dressings with a gentle or thicker adhesive was suggested to reduce the risk of MARSI. A dressing that allows visibility of the incision site, removing the need for opening of the intact dressing, is ideal in practicing UWH where appropriate (Sandy-Hodgetts et al, 2020).
In terms of infection risk, uncontrolled diabetes is a key factor on wound healing, resulting in high rates of infection and other complications. This is one of the risk factors that may be optimised in order to influence patient selection as part of a move towards individualising care and reducing the risk of complications for those patients.
Optimising patient-related risk factors that are modifiable or non-modifiable (Sandy-Hodgetts et al, 2018; 2020) to reduce the risk of surgical wound complications is also ideal, and recommendations are provided elsewhere (WHO, 2016; ERAS Society, 2016).
Properties of the ‘ideal’ dressing
Morgan-Jones et al (2020) previously agreed upon six key requirements of the ‘ideal’ dressing in managing post-surgical incision wounds. The APAC group agreed that these six requirements are all correct according to their local practice.
In addition, one more point was added, based around patient comfort and therefore emphasising the importance of a patient-focused approach.
The updated list of the seven requirements of the ideal dressing is now as follows:
- Flexible (not impede the patient’s movement), providing elasticity to avoid pulling the skin or blistering (e.g. particularly over knee joints)
- Well fixed to the skin on application, even if the wound has been disinfected shortly before
- Absorbent, able to handle exudate
- Skin protective (e.g. reduce the risk of blistering or irritation, not excessively adhesive)
- Waterproof: providing a good seal/barrier function and enabling the patient to shower
- Eliminate dead space where necessary (not leaving a gap between the dressing and the wound bed where blood/exudate can pool, potentially causing maceration and increasing infection risk)
- Patient comfort and atraumatic removal, reducing the risk of compromising skin integrity.