Successful outcomes for patients following surgery are determined by post-surgical incision care including dressing selection and protocol. All clinicians involved in the care of surgical incision wounds should focus on reducing the risk of infection and associated complications (Sandy-Hodgetts et al, 2017; 2018; Morgan-Jones et al, 2019). This consensus meeting was held virtually in January 2022 to examine post-surgical care and dressing selection for surgical incisions closed with primary intention among surgeons working in Poland, Hungary, and the Czech Republic.
The panel follows on from an international consensus panel on the same topic held in July 2019 (Morgan-Jones et al, 2019). There has also been an Asia-Pacific consensus panel (Morgan-Jones et al, 2021a) and a Northern European consensus panel (Morgan-Jones et al, 2021b). The consensus panels have differed in region but have had the same following aims and objectives:
- To clarify global views on incision care and dressing selection in surgical wounds
- To discuss key areas and reach consensus on recommendations
- To discuss findings raised in the previous international reports and agree on the properties of the ‘ideal’ dressing in managing post-surgical incision wounds.
Importance of dressing selection in post-surgical incisions wounds
It is well recognised that dressing selection plays a key role in post-surgical incision care (World Union of Wound Healing Societies [WUWHS], 2016). Post-operative wounds are susceptible to infection and associated complications, and advanced wound dressings play a vital role in protecting the wound during the healing process and in preventing surgical wound complications (SWCs [Box 1]; WUWHS, 2016).
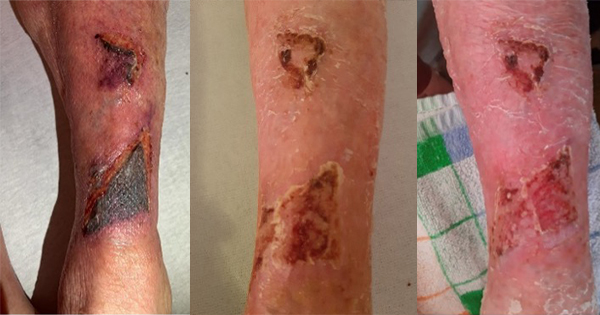
It is important to note that surgical site infection (SSI) is only one type of post-surgical complication: not all complications are related to infection (Sandy-Hodgetts et al, 2020). However, SSIs are among the most common SWC and healthcare-associated infections (HAIs) globally (ECDC, 2016). The burden of SSIs in the EU/EEA was estimated at over half a million cases annually, based on data from the European Centre for Disease Prevention and Control (ECDC, 2013). Across Europe, the overall percentage of SSIs varies from 0.5% to 9.0% depending on the type of surgical procedure – e.g. abdominoplasty in people with obesity has an infection rate of over 30%, and complicated limb traumas requiring surgery have an infection rate of up to 50% (ECDC, 2018).
Currently, SSI prevalence is believed to be underestimated, particularly as hospital infection control programmes do not always include a standardised methodology for post-discharge surveillance (PDS), so the true rate of SSI is likely underreported (WUWHS, 2018). SSI prevalence from the post-acute and home care setting is also lacking. However, good relationships between surgeons and rehabilitation facilities, doctors and physiotherapists can help to support SSI surveillance.
SSIs are associated with longer post-operative hospital stays and may necessitate additional surgical procedures and intensive care, resulting in higher cost and higher attributable morbidity and mortality (Cassini et al, 2016). As a result, the patient should be closely monitored for any signs of local or systemic infection, and treatment plans amended accordingly.
To begin, the team of surgeons reflected on their practice and discussed dressing selection and local protocols in their care setting following surgery. It was agreed that SWCs can be prevented by choosing the right dressing for the right patient, and because there is a certain amount of control over who carries out dressing application and removal. Post-surgical dressing selection is guided by the risk of SWCs, which is dependent on patient factors and surgery type (i.e. general, orthopaedic and trauma).
Following surgery, where there is a very low risk of SWCs, the surgeons discussed the use of a sterile wound dressing when covering the closed incision that:
- Prevents wound contamination
- Maintains a moist wound environment
- Minimises risk of skin damage (e.g. blistering)
- Does not disturb patient mobilisation
- Stays in place for as long as possible, until sutures or staples are removed.
For moderate risk cases following surgery where a longer post-operative hospital stay is required, a dedicated wound dressing that absorbs and retains large volumes of fluid and exudate, allows visibility of the skin and helps reduce the risk of SSIs was proposed, as it can reduce dressing change frequency and dressing-related costs and enable surgeons to observe the surrounding area.
For surgical incisions that are at high risk of SWCs (e.g. a septic or severely contaminated wound), it was agreed that primary delayed suture and/or negative pressure wound therapy (NPWT), or the ‘French Fry’ vacuum assisted closure (VAC) technique (Box 2) may be beneficial in reducing exposure to the environment and risk of infection.
Leaving the dressing in place until patient discharge can prevent wound disturbance and therefore facilitate wound healing (Berg et al, 2019), as well as prevent waste of resources and inefficient use of dressings. Optimising the patient prior to surgery and taking steps during surgery and post-surgery can reduce individual risk of complication (Table 1).
For example, patients receiving planned, elective surgery can be assessed and prepared more accurately than patients requiring emergency surgery. This can include patients showering/bathing on the day of surgery, using a plain or antimicrobial soap/cleanser, and using clippers (rather than a razor) for hair removal prior to the procedure.
Dressing wear time
Many surgeons recommend keeping dressings in place for 7 days post-surgery, although this varies according to local protocol (Brindle and Farmer, 2019). Dressing wear time among the group varied (Box 3); however, they all agreed that the wound status, surgery type and patient cooperation levels can influence dressing wear time.
The group agreed that many dressing change protocols can be dependent on routine habit and a ‘ritualistic’ approach, which has been recognised as a wider issue in wound care (Berg et al, 2019). Hence, a change in mindset is required when approaching incision care that considers the concept of undisturbed wound healing (UWH; Box 4).
UWH requires increased consideration in suitable surgical wounds, particularly in terms of reducing the risk of contamination (Morgan-Jones et al, 2019). The potential benefits of UWH depend on the individual patient and their circumstances; however, in appropriate patients, longer wear time can result in a range of benefits such as (Brindle and Farmer, 2019):
- Optimised healing if the wound remains undisturbed and is on a healing trajectory
- Reduced risk of contamination, potential infection and MARSIs
- Potential cost savings and clinical time.
It was agreed that dressing changes should only be carried out if there is a clinically relevant reason to do so (i.e. the dressing is saturated/leaking; there is excessive bleeding or suspected local/systemic infection; movement is restricted; or the wound is painful or itchy). Other indicators of a necessary or preferred dressing change include potential dehiscence or wound edge deterioration and loss of adherence of the dressing.
Properties of the ‘ideal’ post-surgical dressing
The purpose of a wound dressing for post-surgical incisions is to absorb and retain any leakage, provide ideal conditions for healing and protect the area until the wound is healed. The first international consensus reported six key requirements of an ‘ideal’ dressing in managing post-surgical incision wounds (Morgan-Jones et al, 2019). The Asia-Pacific and Northern European panels included addition requirements that highlighted the importance of patient comfort and usage (Morgan-Jones et al, 2021a; 2021b).
The group of surgeons from Eastern Europe built on the work of the preceding consensus groups to determine the requirement of an ideal dressing for post-surgical incision care.
- Flexible (not impede the patient’s movement), providing elasticity to avoid pulling the skin or blistering (e.g. particularly over joints)
- Well-fixed to the skin on application once the skin is dry after being disinfected and remains adhered if there is sweating (more issue of abdomen)
- Absorbent of wound exudate (retain/lock in fluid; no exudate leakage should occur from the dressing to the periwound skin)
- Protective of the surrounding skin to reduce the risk of blistering or irritation and provide patient comfort, with minimal discomfort or pain during dressing removal
- Waterproof to provide a good seal/barrier function and enable the patient to shower
- Eliminate dead space between the wound bed and wound dressing where necessary to avoid exudate pooling
- Easy to use and remove by patients and all care staff to ensure consistent care
- Transparent dressing borders to allow for observation of the surrounding skin.
Where required by the wound and individual’s circumstances, further specialist dressings may be required – e.g. using closed incision negative pressure wound therapy (ciNPWT) in wounds where heavy exudate/leakage may be an issue.
In addition, ciNPWT should be considered in cases where a high risk of SWC is suspected as a preventive measure (Norman et al, 2020). In the future, smart dressings that can monitor the wound without having to remove the dressing, or that contain smart materials such as stimuli-responsive materials and self-healing materials would be beneficial.
Conclusion
Post-incisional care can vary according to region based on healthcare systems. The group of surgeons working in Eastern European agreed that incision care should focus on reducing the risk of infection and associated complications, and that care should be optimised prior to surgery where possible.
It was also agreed that selecting ‘the right dressing for the right patient’ is essential in surgical incision wounds and that dressings should be left for as long as possible as the principles of UWH are important and necessary for wound healing to progress.
Dressing selection should be carried out according to local protocol, with special consideration given to the wound status, surgery type and individual circumstances, such as patient cooperation levels.