Surgical site infections (SSIs) constitute a considerable burden globally that causes increased morbidity and mortality, especially in developing countries (Allegranzi et al, 2011; Rickard et al, 2020; Sandy-Hodgetts et al, 2022). Even though more than 50% of SSIs are preventable (Umscheid et al, 2011), SSIs are among the most common surgical wound
complication (SWC) and healthcare-associated infections (HAIs) globally (ECDC, 2016). SSI prevalence is believed to be underestimated, as some hospitals may not utilise infection surveillance programmes and those that do may not always include a standardised methodology (Rochon et al 2022). Therefore, it is possible that the occurrence of SSI and surgical wound dehiscence (SWD) is most likely underreported (WUWHS, 2018; Sandy-Hodgetts et al 2018). A cross-sectional observational study at a Saudi tertiary care hospital identified an overall SSI rate of 10.2%; the most frequently isolated
microorganisms were Acinetobacter spp (31.5%), Escherichia coli (25.5%), and Pseudomonas spp (17.9%; Ali Alsareii, 2021).
Additionally, the worldwide increase in antimicrobial resistance poses clinical challenges in the treatment and prevention of SSI and SWD and requires engaging novel approaches in the clinical setting. Antimicrobial stewardship strategies should be in place to reduce the overuse of antimicrobials within post-operative incision management (Sartelli et al, 2016). Contracting an SSI often results in a negative impact on physical and mental health of the individual, a loss of productivity (Badia et al, 2017) and is more commonly associated with longer post-operative hospital stays thay may necessitate additional surgical procedures, resulting in a higher economic burden (Cassini et al, 2016).
Middle East surgical panel SSI prevention may be determined by pre-, periand post-surgical care of the patient, wound
and the care setting. A Middle Eastern surgical expert panel was convened in Dubai, United Arab Emirates, in July 2022, to examine postsurgical care and dressing selection for incisions closed with primary intention. The attending clinicians worked in Kuwait, Saudi Arabia and the United Arab Emirates and represented a range of specialities including, trauma, orthopaedic and reconstructive and cosmetic plastic surgery.
The panel discussed the recommendations of a 2019 international report on post-incision care (Rhidian-Jones et al, 2019) and how they align with local practice. The Middle East surgical panel builds on work by other international surgical panels [Box 1], with the same following aims:
- To clarify local views on post-surgical care and dressing selection for clean surgical incisions closed with primary intention
- To discuss and reach consensus on recommendations for local practice in key areas of optimisation for wound healing pre-, peri- and post-operatively
- To discuss and agree on the properties of the ‘ideal’ dressing in managing post-surgical incisions.
Post-surgical wound care
After surgery, the surgical incision can be categorised using the surgical wound classification system by the Centers for Disease Control and Prevention (2016) depending on the degree of contamination [Box 2]. The panel discussion focussed on clean incisional sites that are closed by primary intention.
Dressing wear time
The degree of contamination and the type of surgery impact on the strategies and treatment plan of the incision. If infection does occur, symptoms often occur within a week. Therefore, daily dressing change is unnecessary as it increases the risk of infection and dressing costs.
Leaving the dressing in place for as long as possible can prevent wound disturbance and facilitate wound healing (Berg et al, 2019). Reduced dressing changes, unless otherwise clinical indicated, may also prevent waste of resources and inefficient use of dressings. Dressing wear time after surgery often varies according to national guidelines, clinician choice, local protocols, and surgical specialty (Brindle and Farmer, 2019). Currently there a paucity in the evidence related to the outcomes associated with early or late dressing removal after surgery (Toon et al, 2015). An observational study has reported that longer dressing wear time following orthopaedic surgery were assoaicted with positive healing outcomes, removing the need for ritualistic and unnecessary dressing changes (Rousseau et al 2021). The potential benefits of undisturbed wound healing (UWH) (Rippon et al, 2012), a relatively new concept in wound management, depends on the patient and their circumstances for suitability. In appropriate clinical situations, longer wear time may result in a range of benefits such as:
- Optimised healing if the wound remains undisturbed and is on a healing trajectory
- Reduced risk of contamination, potential infection and medical adhesive-related skin injuries
- Potential reduction in treatment cost and time (Brindle and Farmer, 2019).
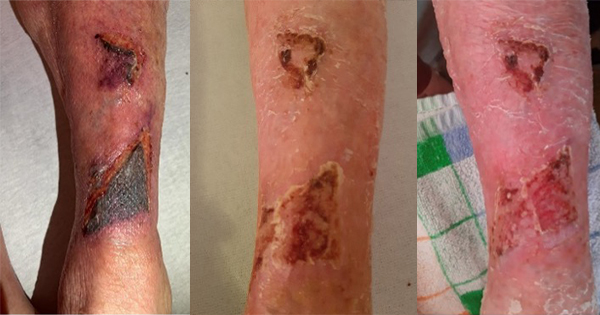
For open or contaminated wounds, or wounds caused by trauma or containing a foreign body, the wound may need to be monitored more often than clean incisional sites. Other reasons to change a wound dressing more frequently are fluid leakage, excessive bleeding, strikethrough or dressing saturation (Morgan-Jones et al, 2019). Potential reasons that dressing change is necessary (or preferred) include:
- Suspected local/systemic infection (e.g. local wound pain, redness, swelling)
- Potential dehiscence or wound edge deterioration
- Loss of adherence of the dressing (i.e. the dressing is peeling off).
Many dressing change protocols can be dependent on routine habit and a ‘ritualistic’ approach, which has been recognised as a wider issue in wound care (Berg et al, 2019). Hence, a change in mindset is required when approaching incision care that considers the concept of undisturbed wound healing. Clinicians involved in the care of surgical incision wounds should focus on reducing the risk of infection and associated complications (Sandy-Hodgetts et al, 2017; 2018; Morgan-Jones et al, 2019). At each patient contact after surgery, as suggested by one of the panel, all clinicians should think: “WHY do I say HI to the wound?”. This has been developed into an acronym to include some of the reasons why a clinician would remove a dressing to inspect the incision [Box 3].
The panel discussed how developing therapeutic relationships with the patient and considering their understanding, knowledge, concerns and wishes, regarding their procedure and aftercare is key to holistic wound healing. The panel also reflected on how, during a dressing change, the patient may be apprehensive of associated pain and may not want to see the wound. It was also emphasised that if the patient does not understand the rationale of treatment, they may not follow advice that will help their incision to heal. Education of the patient regarding the rationale for their wound management plan and providing support to involve the patient may facilitate consistency in care.
Reduce infection risk
To reduce the risk of post-incisional complications, a holistic approach can be taken to optimise person-related risk factors at the pre-, peri- and post-operative stages (ERAS Society, 2016; WHO, 2016; WUWHS, 2018; Sandy- Hodgetts et al 2013; 2019). One of the first steps to reducing SSI risk is to complete a full holistic patient assessment to identify the patient and intraoperative related risk factors relevant to the SSI risk [Box 4].
For patients at high-risk of SSIs, the panel discussed whether they adapted their pre-, peri- or post-operative care. When there is a low SSI risk and the wound is closed by primary intention, the surgeons agreed to using a sterile wound dressing to cover the closed incision. For people who have a moderate or high risk of SSIs, the surgeons would take peri-operative steps to reduce the risk of SSIs, such as closing the wound under minimal or no tension (approximation and not fixation of the wound edges), reducing operation time, reducing the number of people in the operating room, and keeping surgical equipment covered until items are needed. If the patient has a high risk of infection, prophylactic antibiotics or an antimicrobial dressing may be used.
Consistent care
Regardless of the specific dressing and risk management plan, care should be consistent and standardised, and followed by all staff. A challenge of SSI prevention is that many elective surgical procedures are now day cases, so surgeons are in less contact with the patient to review the dressing and ensure SSI prevention strategies are followed. The patient often only returns to the clinic if they experience complications. Also, the patient may be operated on overseas and there may be no plans in place for follow-up care with a specific doctor or hospital or a team local to the patient. Another challenge is conflicting advice from different medical professionals. One way to improve communication between staff could be to write the desired date of dressing change on the dressing itself.
Properties of the ‘ideal’ post-surgical dressing
The purpose of a wound dressing for postsurgical incisions is to absorb and retain any leakage, provide ideal conditions for healing, and protect the area until the wound is healed. The first international consensus reported six key requirements of an ‘ideal’ dressing in managing post-surgical incisions (Morgan-Jones et al, 2019). The Asia-Pacific and Northern European panels included addition requirements for patient comfort and usage (Morgan-Jones et al, 2021a; 2021b). The Eastern European panel added a seventh dressing requirement – transparency – to allow the incision to be visualised (Morgan-Jones et al, 2022).
The surgical group from the Middle East built on the work of the preceding panels to discuss the characteristics of an ideal dressing for clean, closed incisions. Two new characteristics were added – to reduce the risk of complications (e.g. infection and dehiscence) and for the dressing to be cost-effective.
- Flexible (not impede the patient’s movement) to avoid pulling the skin or blistering (e.g. particularly over joints)
- Well-fixed to the skin on application once the skin is dry after being disinfected and remains adhered if there is sweating
- High absorption capability to retain and lock in fluid
- Protective of the surrounding skin to reduce the risk of blistering or irritation and provide patient comfort, with minimal discomfort or pain during dressing removal
- Waterproof to provide a good seal/barrier function and enable the patient to shower
- Eliminate dead space between the wound bed and wound dressing where necessary to avoid exudate pooling
- Easy to use and remove by patients and all care staff to ensure consistent care
- Transparent and absorbent dressing to observe the surgical site, periwound and surrounding skin
- Reduce the risk of complications (e.g. infection, dehiscence).
- Cost-effective.
In the future, smart dressings that can monitor the wound and send readings to an electronic device or that contain smart materials, such as stimuli-responsive materials and self-healing materials, would be beneficial.
Conclusion
Post-incisional care can vary according to region based on healthcare systems. The surgical panel in the Middle East agreed that incision care should focus on reducing the risk of infection and associated complications, and that care should be optimised prior to surgery where possible.
It was also agreed that selecting ‘the right dressing for the right patient’ and understanding the patient’s risk of infection is essential. Dressing selection should be carried out according to local protocol, with special consideration given to the wound status, surgery type and individual circumstances, such as patient understanding, knowledge, expectations and aftercare environment.