Post-surgical incision care is a vital part of the patient journey and must be optimised, particularly in terms of reducing the risk of infection and associated complications. Surgical site infection is a significant issue, affecting approximately 500,000 surgical patients each year in the US, and leading to around 8,000 deaths annually (Najjar & Smink, 2015). In the UK SSI is estimated to affect 6.4% of surgical procedures (Leaper, 2015). Across Europe, the overall percentage of SSIs has been found to vary from 0.5% to 9.0%, depending on the type of surgical procedure – e.g. abdominoplasty in obese patients has an infection rate of over 30%, and the rate in traumatised patients with a Grade 3C open fracture is up 50% (ECDC, 2018).
Dressing selection and protocol plays a key role in post-surgical incision care (WUWHS, 2016). The concept of undisturbed wound healing (UWH) – using a dressing with an increased wear time and keeping the dressing in situ – is a key area of consideration in suitable surgical wounds, particularly in terms of reducing the risk of contamination. Historically, many surgeons recommended keeping dressings in place for 7 days post-surgery, although this now varies according to local protocol (Brindle and Farmer, 2019).
Interestingly, anecdotal evidence from the international group showed a range of opinions in what constitutes the ideal dressing protocol and dressing change time. Taking the individual patient’s needs and preferences into account was agreed to be a key element in dressing selection and the resulting dressing change protocol, with communication and patient education playing a vital role in this process. In addition, concerns around bathing from the patient and family often modify the surgeon’s choices.
The benefits of undisturbed wound healing
It was agreed that UWH is an important topic that requires increased consideration in incision care. While UWH has been practiced sporadically over the years, it is gaining much more attention and is now widely referred to in the clinical management of all wounds (Stephen-Haynes, 2015). In acute wounds such as surgical incisions, protection from contamination is a key factor, which makes UWH of particular relevance (WUWHS, 2016).
While specific timeframes for dressing change – and therefore the selection of appropriate dressings – vary depending on local protocol and individual clinician choice (see Box 1), it was agreed that a change in mindset is required when approaching incision care, giving increased consideration to the concept of UWH.
Regardless of the specific timeframe, a great deal of dressing change protocol can be dependent on routine, habit and a ‘ritualistic’ approach, which has been recognised as a wider issue in wound care (Berg et al, 2019). This means that, instead of dressing change being carried out when it is clinically necessary, dressings may be changed at a particular, predetermined time – not because the dressing necessarily needs to be changed, but because ‘this is when we always do it’. This blanket approach means that the individual requirements of the patient and wound are not taken into consideration, and it may be that the wound is unnecessarily disturbed by dressing change, and healing therefore impeded (Berg et al, 2019).
The group agreed that there are specific criteria which should trigger dressing change (see below), but that otherwise a longer wear time, facilitating UWH, could be considered in suitable patients.
Absolute criteria for dressing change were agreed as:
- Saturation of the wound dressing material
- Excessive bleeding
- Suspected local/systemic infection (e.g. local wound pain, redness, swelling)
- Potential dehiscence.
The individual patient, their wound and overall circumstances should also be taken into account. The patient’s history, any comorbidities and infection risk should be considered as part of a full holistic assessment. Considering the individual needs of the patient and their wound should play a key role in rethinking the ritualistic aspects of dressing change protocol.
The potential benefits of UWH depend on the individual patient and their circumstances. However, in appropriate patients, longer wear time can result in a range of benefits such as (Brindle and Farmer, 2019):
- Healing is optimised if the wound remains undisturbed (unless there is a specific reason to do so)
- Risk of contamination and potential infection is reduced
- Further potential benefits, such as savings in cost and clinician time.
It is also important to consider the patient’s circumstances, individual needs and personal preferences in psychosocial terms, as well as clinical factors (Brindle and Farmer, 2019). For instance, some patients may be nervous of infection or complication, and simply prefer their wound to be looked at more frequently. In patients where UWH is a potentially beneficial option, the patient may need to be educated in the rationale and advantages of this – communication with the patient is of key importance (Blackburn et al, 2018). Similarly, cultural and individual differences may come into play, and some patients may prefer their wound to be covered even when it is not clinically necessary. Taking into account these different requirements for individual patients should be a part of making an appropriate dressing selection. On the other hand, patients will appreciate the reduced pain associated with diminished frequency of dressing changes.
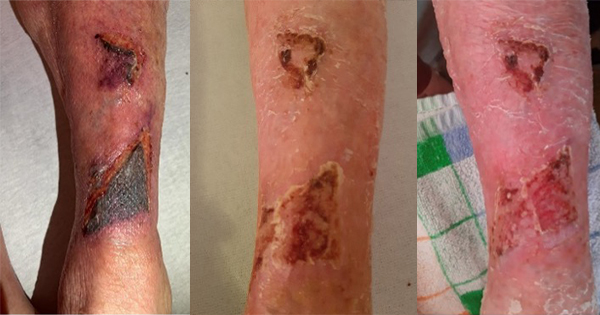
It should also be emphasised that monitoring – and changing the treatment plan where necessary – is vital. For instance, if the dressing becomes saturated then it should be changed regardless of the planned timeframe. To avoid the risk of maceration or damage to the surrounding skin, fluid should not be in direct contact with the patient’s skin (although this may be mediated by the dressing choice).
The risk of infection should also be considered, with the patient monitored for any signs of local or systemic infection, and treatment plans amended accordingly. Anecdotally, it was suggested that routine dressing change in the early stages of healing may be with the aim of observing signs of potential infection. However, it is worth noting that in the first 48 hours post-surgery, signs of superficial infection would not yet be visible, and any inflammation observed is likely to be normal at this stage rather than a sign of infection, so it is important not to conflate the two (WUWHS, 2016). Cited data states that the majority of SSIs become apparent between the 5th and 10th post-operative day (most patients are discharged by this time). However, when prosthetic implants are in place, this can occur several months after the operation (NICE, 2019).
The group agreed that the ‘absolute indicators’ listed above – e.g. saturation or suspected infection – should trigger immediate dressing change. Other factors should be considered of comparatively relative importance, and can trigger dressing change at the clinician’s discretion, taking into account individual needs and cultural or circumstantial preferences.
Dressing properties
The following were agreed to be requirements of the ‘ideal’ dressing in managing post-surgical incision wounds:
- Flexible (not impede the patient’s movement), providing elasticity to avoid pulling the skin or blistering (e.g. particularly over knee joints)
- Well fixed to the skin on application, even if the wound has been disinfected shortly before
- Absorbent, able to handle exudate
- Skin protective (e.g. reduce the risk of blistering or irritation, not excessively adhesive)
- Waterproof: providing a good seal/barrier function and enabling the patient to shower
- Eliminate dead space where necessary
Flexibility was identified as an issue of key importance, both in terms of skin protection (i.e. not causing further damage, such as blistering or tension injuries) and patient comfort and mobility. Medical adhesive-related skin injury (MARSI) is prevalent, under-recognised and preventable, so flexibility and skin-protective properties are of utmost importance (Wounds UK, 2016). As well as dressing selection, care should be taken with dressing change technique to ensure that the risk of MARSI is reduced as far as possible.
There was some debate over the issue of using antimicrobial dressings. In selected cases where infection risk is elevated, an antimicrobial dressing (e.g. silver) may be used as standard. However, it was emphasised that antimicrobial dressings can be overused unnecessarily, and there must be a clear evidence-based rationale before any antimicrobial dressing is used prophylactically. In general on well co-apted/closed skin there is very little data to support the application of a topical antimicrobial.
Where required by the individual wound and patient circumstances, it should be noted that further specialist dressings may be required – e.g. using negative pressure wound therapy (NPWT) in wounds where heavy exudate/leakage may be an issue. Whether this may increase peri-incisional lymphatic clearance or improve local blood flow remains subject to further assessment. It should be noted that, in some instances, the closed wound should also be protected by the application of a preventive closed incision negative pressure therapy.
In addition to the other dressing properties discussed, it was agreed that visibility of the wound through the dressing (i.e. dressing transparency) may or may not be possible depending on the circumstances of the individual wound (e.g. wounds with high volume of exudate). However, in suitable wounds, dressing transparency may be beneficial in the management of post-surgical incision wounds, which may warrant further research.
Overcoming barriers to undisturbed wound healing
There is a need to convey the message that there is no need to disturb the wound unless there is a specific clinical reason to do so. If dressing selection is made with this in mind, this should be considered throughout the process, ensuring that dressings are used efficiently.
Otherwise, there is a risk that dressings may be selected that have the capability of sustained wear, but may still be unnecessarily changed purely for ritualistic reasons – thus wasting resources and using dressings inefficiently.
Accordingly, education about dressing capability and the potential benefits of UWH for appropriate patients is key. Clinicians need to be aware of the rationale and benefits, and this also needs to be communicated effectively to the patient.
Summary
While protocols and preferences may vary, the expert group agreed that UWH is a topic of growing importance. Dressing change ‘ritualism’ has been identified as a wider issue in wound care, and this particularly applies to post-surgical incision wounds, where pre-set schedules may be in place regardless of individual clinical need.
Incision care is an area with specific dressing needs, and consideration needs to be given to the patient, the wound and the individual circumstances.