The aim of these meetings was to examine post-surgical care and dressing selection for surgical incisions closed with primary intention among surgeons working in different geographical regions, for Class I procedures only (CDC, 2016). The consensus panels differed in each region but each one had the same overall aims and objectives:
- To clarify global views on incision care and dressing selection in surgical wounds
- To discuss key areas and reach consensus on recommendations
- To discuss findings raised in the previous international reports and agree on the properties of the ‘ideal’ dressing in managing post-surgical incision wounds.
While there were some geographical variations in best practice, there were broad areas of agreement in the aims when treating incisional wounds.
The importance of dressing selection in surgical wounds
Post-operative wounds may be susceptible to infection and associated complications, and advanced wound dressings play a vital role in protecting the wound during the healing process and in preventing surgical wound complications (SWCs) (WUWHS, 2016).
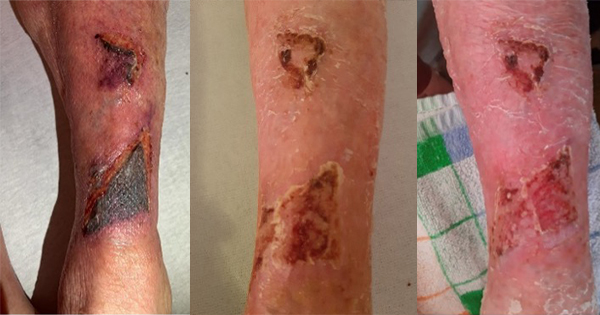
The term SWCs is a broad term that incorporates specific diagnoses such as surgical wound dehiscence, surgical site infection (SSI), hypergranulation, peri-wound maceration, scarring and medical adhesive-related skin injury (MARSI; Box 1; Sandy-Hodgetts et al, 2020).
Surgical site infections are among the most common SWC and healthcare-associated infections (HAIs) globally (ECDC, 2016). The burden of SSIs in the EU/EEA was estimated at over half a million cases annually, based on data from the European Centre for Disease Prevention and Control (ECDC, 2013). Across Europe, the overall percentage of SSIs varies from 0.5% to 9.0% depending on the type of surgical procedure – e.g. abdominoplasty in people with obesity has an infection rate of over 30%, and complicated limb traumas requiring surgery have an infection rate of up 50% (ECDC, 2018).
Currently, SSI prevalence may be underestimated, as post-discharge surveillance programmes are sporadic and in some cases absent (Rochon et al 2020; Sandy-Hodgetts et al 2022; Fletcher et al 2022). Moreover, standardised methodologies for surveillance that are consistent in definitions, methodology and data capture that allow for pooling of data are in its infancy, hence a deficit in the known burden of this type of wound outside of the acute care setting. Therefore, the true rate of SSI and SWD may be underreported (WUWHS, 2018).
SSIs are often associated with longer post-operative hospital stays, may necessitate additional surgical procedures, may require intensive care, and can result in higher cost and higher attributable morbidity and mortality (Cassini et al, 2016; Baida et al, 2017; Totty et al, 2021).
Successful outcomes for patients following surgery are multi-factorial, with dressing selection and post-operative care protocols a key part of the patient’s surgical journey. All clinicians involved in the care of surgical incision wounds should focus on reducing the risk of infection and associated complications (Sandy-Hodgetts et al, 2017; 2018; Morgan-Jones et al, 2019). The international groups reached consensus around best practice in caring for incisional wounds and selecting products according to the patient’s needs.
Properties of the ideal dressing
In the meetings, the surgeons reflected on their practice and discussed dressing selection and local protocols in their care settings following surgery.
Dressing selection plays a key role in post-surgical incision care (WUWHS, 2016). The purpose of a wound dressing for post-surgical incisions is to absorb and retain any leakage, provide ideal conditions for healing and protect the area until the wound is healed.
There is considerable discourse regarding the efficacy of wound dressings for prevention of SSI (Dumville et al, 2016; WHO, 2016; Sandy-Hodgetts, 2017). Protection of the incision site is of key importance, particularly in managing the risk of SSI and SWD. More importantly, for improved patient wellbeing and outcomes, is the ability to create an optimal wound healing environment.
Following a Class I procedure where risk of SSI may be low or negligible, the use of a cover dressing with the following properties is ideal:
- Prevents wound contamination
- Maintains a moist wound environment
- Minimises risk of skin damage (e.g. blistering)
- Does not disturb patient mobilisation
- Stays in place for as long as possible, until sutures or staples are removed.
For moderate risk cases, following surgery where a longer post-operative hospital stay is required, a dedicated wound dressing that absorbs and retains large volumes of fluid and exudate, allows visibility of the skin was proposed, as it can reduce dressing change frequency and enable surgeons to observe the surrounding area, leaving the dressing in situ.
The first international consensus reported six key requirements of an ‘ideal’ dressing in managing post-surgical incisions (Morgan-Jones et al, 2019):
- Flexible (not impede the patient’s movement), providing elasticity to avoid pulling the skin or blistering (e.g. particularly over knee joints)
- Well fixed to the skin on application, even if the wound has been disinfected shortly before
- Absorbent, able to handle exudate
- Skin protective (e.g. reduce the risk of blistering or irritation, not excessively adhesive)
- Waterproof: providing a good seal/barrier function and enabling the patient to shower
- Eliminate dead space where necessary.
The Asia-Pacific and Northern European panels discussed additional requirements for patient comfort and usage (Morgan-Jones et al, 2021a; 2021b). The Asia-Pacific panel discussed the potential for an additional consideration – transparency of dressing borders – to allow the surrounding skin to be visualised (Morgan-Jones et al, 2022). However, there was some debate as to whether there is a benefit to the wound being visible (i.e. through the use of a transparent dressing pad). It was generally agreed that for some very low-exuding wounds this might be relevant; however, it was also stated that some patients may become more anxious if they are able to see the wound.
The Middle East panel added two new characteristics – to reduce the risk of complications (e.g. infection and dehiscence) and for the dressing to be cost-effective. Additionally, the African panel suggested that the dressing should be as small as possible while being suitable for the size of the patient’s wound; if a large dressing is placed over a wound, the patient will assume their wound is relatively large in size and may be more anxious than necessary about their wound.
Dressing wear time
Dressing wear time among the groups varied; however, they all agreed that the wound status, surgery type and patient cooperation levels can influence dressing wear time. It was also agreed that it is important to choose a dressing that can manage exudate and afford extended wear time wherever possible.
The standard dressing wear time for surgical sites varied among the panels based on the surgery type, local protocol and clinician choice (Box 2). However, what remained constant was the importance of consistency and standardisation in care. Regardless of the specific protocol for dressing changes, it is vital that the protocol is followed by all staff and that it is individualised for the person at the centre of care.
Undisturbed wound healing
A great deal of dressing change protocol can be dependent on routine, habit and a ‘ritualistic’ approach, which has been recognised as a wider issue in wound care (Berg et al, 2019). This means that, instead of dressing change being carried out when it is clinically necessary, dressings may be changed at a particular, predetermined time – not because the dressing necessarily needs to be changed, but because ‘this is when we always do it’. This blanket approach means that the individual requirements of the patient and wound are not taken into consideration, and it may be that the wound is unnecessarily disturbed by dressing change, and healing is therefore impeded (Berg et al, 2019).
Across the groups, it was agreed that UWH is an important topic that requires increased consideration in incision care. While UWH has been practiced sporadically over the years, it is gaining much more attention and is now widely referred to in the clinical management of all wounds. In acute wounds such as surgical incisions, protection from contamination is a key factor, which makes UWH of particular relevance (WUWHS, 2016).
The potential benefits of UWH depend on the individual patient and their circumstances. However, in appropriate patients, longer wear time can result in a range of benefits such as (Brindle and Farmer, 2019):
- Healing is optimised if the wound remains undisturbed (unless there is a specific reason to do so
- Risk of contamination and potential infection is reduced
- Further potential benefits, such as savings in cost and clinician time.
While specific timeframes for dressing change – and therefore the selection of appropriate dressings – vary depending on local protocol and individual clinician choice, it was agreed that a change in mindset is required when approaching incision care, giving increased consideration to the concept of UWH.
There are, of course, cases when promoting UWH is not suitable; fluid leakage, strikethrough or dressing saturation are reasons to change the wound dressing (Morgan-Jones et al, 2019). Potential indicators that dressing change is necessary (or preferred) include:
- Saturation of the wound dressing
- Dressing leakage
- Excessive bleeding
- Suspected local/systemic infection (e.g. local wound pain, redness, swelling)
- Potential dehiscence or wound edge deterioration
- νLoss of adherence of the dressing (i.e. the dressing is peeling off).
Region-specific considerations
There are some region-specific considerations in dressing selection and wound healing, including factors around the dressing or cultural considerations. For example, in some humid/tropical climates, waterproof dressings are very important. Patients travelling long distances can also be an issue in dressing selection and change frequency. It is important that patients can be confident they have the information and resources they need when they are far from the hospital.
Patient optimisation before and after surgery utilising the Enhanced Recovery After Surgery (ERAS) protocols is used in some areas, which include post-surgery dressing requirements (ERAS Society, 2016). While it is not universally embedded in clinical practice, early adopters have seen improved outcomes (Gustafsson et al, 2013; Kaye et al, 2019).
It was agreed that good pre-operative assessment can generally improve outcomes and the WHO surgical checklist (WHO, 2020) is also used in some settings. It was agreed that using checklists and ensuring that a specific staff member takes responsibility for checklists, and that senior staff are vigilant in standard-setting, can have a positive effect.
It is also important to note that product availability across differing geographic regions can present issues for dressing choices in clinical management, as not all dressings are widely available in all care settings. Cost is also a consideration.
Summary and key points
Post-incisional care can vary according to region based on healthcare systems. Incision care should focus on reducing the risk of infection and associated complications, and that care should be optimised prior to surgery where possible.
Dressing selection should be carried out according to local protocol, with special consideration given to the wound status, surgery type and individual circumstances, such as patient cooperation levels. The groups agreed that incision care is an area with specific dressing needs as outlined by the ‘ideal’ dressing requirements.
It was agreed that selecting ‘the right dressing for the right patient’ is essential in surgical incision wounds and that dressings should be left for as long as possible as the principles of UWH are important and necessary for wound healing to progress.
Dressing change ‘ritualism’ has been identified as a wider issue in wound care, and this particularly applies to post-surgical incision wounds, where pre-set schedules may be in place regardless of individual clinical need.
Although post-incisional care may vary across different geographical regions, the groups agreed that consistent care and standardisation across care settings; individual optimisation
pre-, peri- and post-surgery; education and training of staff; and access to the surgical team are vital to improving outcomes for people with incisional wounds.
To improve outcomes for incision care, an appropriate dressing needs to be selected that meets the requirements discussed, and to ensure that dressings are changed only when clinically necessary, rather than in a ‘ritualistic’ way, promoting UWH.