Venous leg ulcers are one of the most common type of chronic lower extremity ulcers. They can be slow to heal and are both painful and costly (Bonkemeyer Millanet al, 2019). Venous ulcers affect a large portion of the adult population and their prevalence and incidence increases with aging and higher prevalence of associated chronic conditions, such as arterial hypertension and diabetes mellitus (Abbade et al, 2020). There is a high incidence of patients with recurrent episodes of prolonged ulceration caused by venous hypertension or stasis (Norman et al, 2018).
Compression therapy is the first-line treatment, but a range of dressings and topical treatments are also used. Along the measures to reduce the effects of venous hypertension, local treatment of the wound, such as debridement and dressings, systemic drugs, and complementary measures are also used (Abbade et al, 2020; Bowers and Franco, 2020). Venous ulcers are complex clinical situations and the importance of this type of injury and its influence on the physical and psychosocial behaviour of the patient, specially the diabetic patient, justifies any treatment attempt (Norman et al, 2018; Bonkemeyer Millan et al, 2019; Abbade et al, 2020).
An antiseptic ointment for dental implants and surfaces (Proheal – BiomacMed, Juiz de Fora, MG, Brazil) composed of triiodomethane and calendula, has shown consistent long-term results in microbiological control and tissue regeneration in the oral cavity (Cruz and Castro, 2001; Cruz et al, 2013; Pereira et al, 2017). The product is an antiseptic that occupies the gaps in the implant/component interconnections, preventing the colonization and transit of bacteria (do Nascimento et al, 2019). Likewise, it fills in surface roughness and forms a protective film, exerting an antifouling action, preventing biofilm formation on exposed surfaces in the oral environment. It also acts as a cell stimulator, favouring tissue healing of the oral mucosa and gingival tissues adjacent to implants and prostheses (Cruz et al, 2013).
This work aimed to report a case successfully treated with Proheal antiseptic ointment. This case report follows the CARE guidelines (Riley et al, 2017).
Case presentation
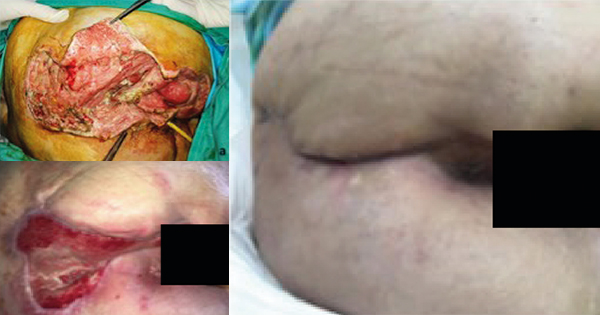
A 75-year-old, white woman, with hypertension and type 2 diabetes for about 45 years, had a chronic venous ulcer (CEAP C6) in the ankle region that had been present for 40 years. The wound measured approximately 6 cm × 9 cm [Figure 1], presented no signs of infection, and was resistant to previous treatments.
The patient reported that the ulcer started as a small wound and it grew over the years. Depending on the treatment, the ulcer would reduce in size, but never closed. The size remained practically the same throughout the years. Previously the patient used antibiotics, Unna Boot dressings (inelastic compression therapy) and baths with the herbal treatment barbatimão (Stryphnodendron adstringens).
According to the patient’s assessment of pain, she described moderate to severe pain to the touch (Visual Analog Scale [VAS] 5-8), moderated and constant spontaneous pain (VAS 3-4), which occasionally remained light (VAS 1-2). The presence of the ulcer and the constant pain interfered with her social life, generating psychosocial consequences.
Her past medical history included hypertension management with losartan, atenolol, furosemide and amlodipine, diabetes management with glimepiride and metformin, and other medications, including atorvastatin, bromazepam, coumarin and troxerutin. The patient maintained the blood pressure and diabetes under control throughout the treatment. She signed a consent form and was verbally informed about the research and the methodology to be applied.
Treatment
The medication was applied once a day at the patient’s home, by family members, after cleaning with tap water. The patient was instructed to sunbathe the wound for at least 15 minutes daily. The family members responsible for the treatment were asked to gently massage around the ulcer, following a podalic-cranial direction, to favour venous return. During the study period, the patient suspended all other treatments for the ulcer.
Progression
The ulcer showed a constant clinical detectable closure from the second day onward. The patient declared that the pain disappeared almost entirely after the second application, and her emotional state was visibly improved.
The aspect of the lesion continued to change favourably until day 65. An allergic reaction occurred, which was suspected to be an allergy to triiodomethane. There was pruritus, redness, swelling and pain in the ulcer region [Figure 2]. Proheal was suspended, and the allergic reaction was treated with hydrocortisone ointment, dexchlorpheniramine and betamethasone, administered twice a day for 5 days.
On day 84, the wound care was resumed, with hygienic care, massage, sunbathing and application of a new ointment formulation without triiodomethane.
At this time, the ulcer had evident signs of healing. The medication was maintained, with the same application regimen, for another 60 days, without any adverse reaction. The wounds was completely healed on day 143 [Figure 3]. The patient was followed up for another 16 months, during which time the tissues remained healthy, despite the changes in the epidermis colour [Figure 4].
Discussion
This case showed relevant results of a drug transposed from one type of application to another. This transposition is justified since it showed satisfactory responses in the oral mucosa, by controlling the infection and enhancing the tissue reaction to healing.
The case study eliminated variables capable of affecting ulcer tissue response, such as other local or systemic drugs. A weakness of this case study may be that, during treatment, the patient did not attend any medical appointments and was cared for exclusively by her family members at home, guided by the researchers. This conduct may have created biases and lengthened the treatment time, but, at the same time, it reinforced the results, as the treatment was performed without the involvement of healthcare professionals. Sunbathing and the requested massage were considered an adjuvant. However, these factors may be included, as variables, in new studies.
Standard treatments for venous ulcers consists of local wound care and removal of the effects of venous hypertension. General principles for local management of chronic wounds are based on the TIME principles, as well as cleaning, debridement, dressings and biofilm control (Abbade et al, 2020; Bowers and Franco, 2020). Prior to the treatment described, the patient had used several strategies, including compression therapy with an Unna Boot dressing (inelastic compression therapy), which was inefficient. Different treatments and dressings for venous ulcers have been tested, but many still with controversy or insufficient evidence for their adoption (O’Meara et al, 2014; Norman et al, 2018; Bonkemeyer Millan et al, 2019; van Netten et al, 2020).
The results using the Proheal ointment were satisfactory, with complete healing of the ulcer, in a relatively short period for this type of lesion when compared with traditional treatments (Norman et al, 2018; Bonkemeyer Millan et al, 2019). However, there is no guarantee that these results will repeat in other cases. The importance of this type of injury and its influence on the physical and psychosocial behaviour of the diabetic patient justifies the treatment attempt.
The role of topical antiseptics and antibiotics in managing venous leg ulcers remains unclear (O’Meara et al, 2014). No work found in the literature reported the use of drugs similar to those used in this case, separately or in combination. The results obtained in this case do not support the hypothesis that antiseptic Proheal is effective in treating these ulcers. However, we encourage additional trials to be performed with the medication.
Conclusion
Despite the complexity of venous ulcer management, the treatment of this case using the antiseptic Proheal, was satisfactory, with a favourable conclusion and long-lasting results. The results encourage clinical trials with the ointment to generate evidence for its use in skin ulcers or other types of wounds.
Declaration of interest
Authors José Maria Almeida Castro and Mauro Cruz developed the ointment in the 1990s. The other authors are from the research centre that developed the ointment and participated in publications about the product.
Acknowledgements
The authors thank Dr Clóvis da Cruz Reis, whose indomitable spirit and scientific career led the Clinest-Clinical Center of Research in Stomatology to this level.