Early identification of changes to the skin is one of the most important tools to protect patients who are at risk of developing pressure ulcers (Haesler, 2019). Recognition and appropriate management of early signs of pressure damage can prevent the development of more advanced categories of pressure ulcers with significant benefits for patients, as well as for nursing teams who otherwise have to regularly treat the wound (Jackson et al, 2018; National Wound Care Strategy Programme, 2021). Traditionally, training materials and guidance on the early identification of pressure ulcers has focused on paler skin, including the ‘React to Red’ (React to red skin, no date) campaign with guidance on changes to look out for and sample images based on patients with White skin tones (Oozageer Gunowa et al, 2021).
Birmingham Community Healthcare NHS FT provides community and specialist services within Birmingham and the West Midlands. The Trust delivers over 100 clinical services, out in peoples homes and in over 300 hospitals, health centres and clinics. The Trust provides services for adults, children, people with learning disabilities, those with rehabilitation needs and also dental services.
Birmingham Community Healthcare
The city is very diverse; the 2021 census results shows 48.6% of residents reporting their ethnicity as White, 17% as Pakistani, 5.8% as Indian, 4.2% Bangladeshi and 3.9% Caribbean.
The Trust employs just over 5,000 staff and sought feedback from staff from the Adult Specialist Rehabilitation (ASR) Division (providing in-patient services) and the Adult Community Services (ACS) Division (providing Community Nursing services).
In the ACS division, 97.66% of staff have reported their ethnicity on the Trust’s ESR portal. Of those, 63.5% reported their ethnicity as White with 36.5% belonging to a Black, Asian or minority ethnic (BAME) group. With the ASR division 98.8% of staff have reported their ethnicity on the Trust’s ESR portal. Of those, 59.1% reported their ethnicity as White with 40.9% belonging to a BAME group.
Data on patient ethnicity have a lower level of accuracy with overall 93.9% of ASR patients and 93.1% of ACS patients having ethnicity recorded based on unique patients seen in February 2023. Of the unique patients with a known ethnicity seen by the two divisions in that month, 56.5% of ASR referrals were for White patients, while 71.3% of referrals to community services were for White patients. This highlights that patients seen in adult services and particularly those with a focus on frailty and support to older patients are not representative of the overall demographics of the city.
Aim
This project aimed to survey staff working with pressure ulcers to understand how confident they are of their ability to identify early signs of pressure damage and to survey what advice and guidance they felt would be helpful in addressing pressure ulcers in patients with dark skin tones.
Design
Following the review of the Trust’s pressure ulcer data, 2021/22 survey responses were collected in two stages. A Smart Survey portal was set up to collate anonymous responses in March 2022 in community settings and specialist inpatient wards. Additionally, the first author took paper versions to groups of community nurses as they were waiting for access to the smart portal, which had not been granted at the point in time that the initial sessions had been arranged. These paper responses were collated in November 2021.
Review of pressure ulcer data 2021/22
The authors reviewed data from the Trust’s Datix incident report management system to understand the ethnic breakdown of the patients for all pressure ulcers which were recorded by the ACS and Adult Specialist Rehabilitation Services on the Trust system from April 2021 to March 2022. This data included pressure ulcers developed in Trust care and those that were treated but had developed under the care of other providers. The data cover both community and in-patient adult services.
In total, 3,391 pressure ulcers were reported. While category 1 pressure ulcers would provide further information on early stage identification of pressure ulcers, on review of the Trust’s data for these categories, is was deemed that the data completeness was not adequate to provide a breakdown of ethnicity. The national Safeguarding Adults Protocol indicates that single category/grade 1 and 2 pressure ulcers “must be considered as requiring early intervention to prevent further deterioration of damage”. (Department of Health and Social Care, 2018) and the Trust’s standard practice requires staff to record for more severe categories only. This has been acknowledged as a limitation of reporting on category 1 pressure ulcers in a previous study (Smith et al, 2016).
The data suggest that patients who report their ethnicity within one of the categories included in Black or Asian have higher representation with more severe categories of pressure ulcer and specifically grades 3 and 4. Pressure ulcers with no patient ethnicity recorded against them (9.29% of the total) were excluded and then White patient outcomes were compared to patients declaring any other BAME category [Figure 2].
Participants
Forty staff responded to the smart survey and fifty-seven staff completed paper surveys giving a total of 97 responses [Table 1]. All were employees of Birmingham Community Healthcare Foundation Trust at the point when responses were submitted.
The smart survey responses were reported as an Excel Spreadsheet. A further Excel spreadsheet in a similar format was created and the results of the paper survey were manually entered into this spreadsheet. To maintain confidentiality each paper return was marked with a unique reference which was also recorded on the spreadsheet. The returns were summed to calculate participant ethnicity and to understand the experience of the respondents and how these factors related to confidence when managing pressure ulcers in patients across a range of skin tones. The 60% White staff who replied to the digital survey and 54.4% who replied to the paper survey are broadly representative of the overall proportion of White staff employed in the divisions surveyed suggesting that the data had no overall bias towards BAME or White staff.
Staff were asked to self-report their experience of how many years they had worked with pressure ulcers [Table 2].
Data collection
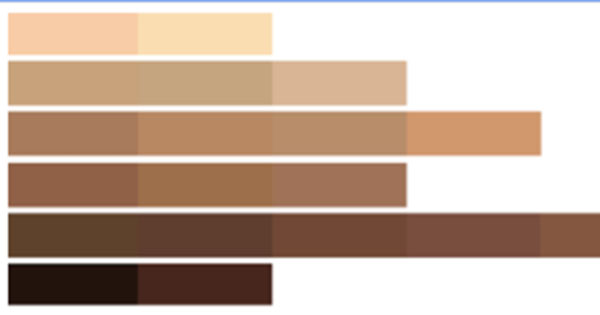
Respondents to the survey were shown a range of skin tones and asked: ‘How confident are you in identifying signs of early-stage pressure damage in patients with different skin tones?’ Staff were then asked to give a rating from 10 (very confident) to 1 (not very confident) against each of the following colour bands.
The colour bands are taken from a tool developed by Ho and Robinson (2015) [Figure 3]. The use of these colour bands is important as patient reported ethnic categories will include a wide range of skin tones (Wounds UK, 2021). To avoid ambiguity staff were asked to focus on an actual skin tone rather than being asked to imagine a representative skin tone based on ethnicity. Staff were asked which indications of pressure damage they used when looking for early signs of pressure damage among people with dark skin tones and finally were asked for any suggestions they have for support to improve the identification of pressure damage for patients with dark skin.
Unfortunately, due to an error in the smart survey set up, respondents to the electronic survey were only asked about skin tones 1–5 in the image above. As a result of this inconsistency, the digital and paper data have been presented separately. However, consistent questions were asked through both methods of data collection about the signs that staff use and, therefore, this data has been analysed as a single dataset.
Staff ethnicity and confidence
The data was analysed to understand how confident staff reported themselves to be when identifying early signs of pressure damage in patients across a range of skin tones. For each skin tone, the mean average confidence of all respondents from the paper survey and then separately the smart survey was calculated. To explore how staff ethnicity affects confidence, the data from the smart survey were summed to establish the overall mean average confidence of all respondents and separately those who reported their ethnicity as Black, White, Asian, Mixed and ‘Not stated’. The same process was carried out on the paper responses.
Ethnicity and confidence
— smart survey
The 40 smart survey responses report reducing confidence as the patient’s skin tone gets darker. Overall, the average response was a confidence rating of 7.63 for the palest skin and 5.43 for the darkest skin. Respondents who gave their ethnicity as Black were somewhat more confident than White respondents in identifying pressure damage on all grades of skin shown. However, both groups show a proportionally very similar reduction in confidence as the skin gets darker.
Ethnicity and confidence — paper respondents
The 57 paper survey responses report reducing confidence as the patient’s skin tone gets darker. Overall, the average response was a confidence rating of 8.13 for the palest skin and 3.04 for the darkest skin. Respondents who gave their ethnicity as Black were somewhat more confident than both Asian and White respondents in identifying pressure damage on all grades of skin shown. White respondents showed slightly lower confidence and Asian respondents were overall closer to the mean average. However, all groups show a very similar and sizable reduction in confidence as skin gets darker.
Confidence and experience
In order to explore how staff experience affects confidence, data were taken from the smart survey and the mean average confidence was then calculated separately for respondents reporting 0–5, 6–10, 11–15 and 16 or more years’ experience. The same analysis was carried out for the paper survey responses.
Experience and confidence
— smart survey
The 40 smart survey responses report reducing confidence as the patient’s skin tone gets darker. Staff are generally more confident in their ability to detect pressure ulcers in all skin tones with increased experience although the longest serving staff are interestingly slightly less confident than those in the 11–15 years’ experience bracket. All experience brackets report reduced confidence with darker skin tones.
Experience and confidence
— paper survey
There existed a limited link between confidence and experience. While the least experienced staff have the lowest levels of confidence, staff in the 6–10 years bracket report highest levels of confidence. However all experience brackets report reduced confidence with darker skin tones. Overall, the data show a significant drop in confidence towards the management of patients with darker shades of skin with an overall confidence of 8.22 relating to skin tone one (the palest tones) dropping to an average of 3.14 for skin tone 6 (the darkest tones).
Analysis of confidence data
Both smart survey and paper results show significant drops in confidence, and it is notable that the paper results show a much sharper drop in confidence than the smart survey results. There may be a number of factors behind this difference.
The paper survey respondents may have been more confident of anonymity and therefore more negative about their own abilities than the smart survey respondents. Paper returns were shown an additional skin tone shown above as band number 6 while smart survey respondents only saw bands 1 to 5. The additional consideration of skin tone band 6 possibly led to decreased confidence in respondents throughout other bands.
Staff who returned the paper surveys also had an in person briefing to introduce the aims of the project which included time for questions. Staff who returned the online forms were given a short introductory paragraph about the project. It is possible that this different approach also affected confidence of the respondents.
It is notable that staff across a range of ethnicities and a range of experience levels reported decreasing confidence. The drops in confidence reported, especially from the paper survey are clearly significant and a cause for concern requiring a response involving additional training and support. The paper respondents were overall somewhat less experienced than the smart survey returns.
Current methods of assessing skin for tissue damage
Staff were asked which possible signs of tissue damage they were using when assessing patients with dark skin tones. Staff replied as shown in Figure 4 with all options being currently used by a majority of staff based on the Wounds UK (2021) Best Practice Statement ‘Addressing Skin Tone Bias in Wound Care: Assessing Signs and Symptoms in People with Dark Skin Tones’.
Targeted tools and training
Staff were also asked if they had received specific training on the assessment of tissue damage in patients with dark skin tones. Overall, just over 5% reported having received specific training on this subject matter (although the providers of this training were not specified). BAME staff were more likely to report having received specific training with 13.64% of Black staff (3 of 22) and 27% of Asian and Mixed Race Staff (3 of 14) reporting that they had received specific training. Just 3 of 55 White respondents (5.5%) reported receiving specific training. However, levels of all staff receiving specific training are low and unlikely to account for differing levels of confidence.
A sizable majority of all staff felt that specific tools to assess dark skin tones would be appropriate with overall 90.7% of staff (88 of 97 responses) agreeing that this would be appropriate. Among Black staff approval was even greater with 100% of the 23 Black staff who responded saying that a specific tool would be appropriate.
Additional ideas and suggestions
Respondents to the survey were also asked what other changes to skin they have seen in patients with tissue damage and dark skin tones and finally what they would find useful to help clinicians in assessing pressure damage in people with dark skin tones.
Many staff reported that damaged skin would appear darker than the surrounding skin and a few referred to heat, pain and dryness or changes in texture as additional signs. These factors should be considered for inclusion in new training on pressure ulcer prevention (Dhoonmoon et al, 2021).
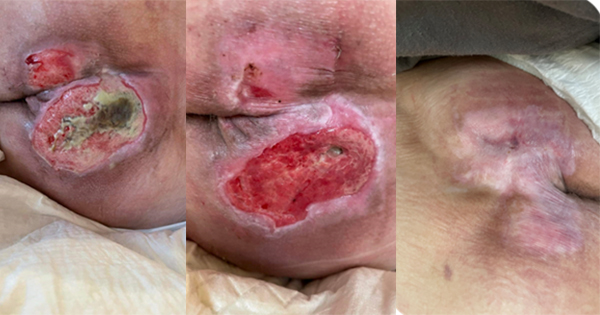
By far the most common suggestion or request was for visual guides with photographs showing pressure damage on dark skin with some staff noting that this should be backed with specific training. Some noted that all the examples they had seen in previous training were of damage to pale skin.
Others highlighted:
The importance of speaking to patients and carers to ask them if anything had changed on their skin or if they had any pain
That torches would be useful (noting low / poor lighting in many homes)
The use of digital visual records as a reference aid.
Limitations
Data are based on pressure ulcers and not patients and so some patients will be included more than once. For 9.29% of all pressure ulcers (315 individual pressure ulcers), there was no patient ethnicity recorded. Data do not include information on category 1 — those most difficult to identify in dark skin tones.
It is important to recognise that the data are based on patient stated ethnicity and each category will include a wide range of skin tones. This data suggest a correlation between darker skin tones and worse outcomes as far as the development of more advanced pressure ulcers is concerned.
Recommendations
To explore the feasibility of implementing and piloting digital visual records through the use of a photo application in order to provide a visual reference and increase the opportunities for earlier identification and detection of category 1 and 2 pressure ulcers in people with dark skin tones within tissue viability and district nursing teams based on staff feedback.
New training has been developed that is specific to pressure damage and people with dark skin. The delivery of this training commenced in 2021 for anyone who is involved in skin inspection, this includes band 5–8 Pressure Ulcer competencies and is based on recommendations from the following clinicians and researchers that placed an emphasis on increasing the knowledge, understanding and confidence of how some conditions can present differently in darker skin tones (Bates-Jensen, 2009; Dhoonmoon et al, 2021; Haesler 2014; Mukwende, 2020; Oozageer Gunowa et al, 2020).
The NHS England PU Core Curriculum does not provide any specifics and the National Wound Care Core Capabilities Framework for England (Skills for Health, 2022) does not mention inclusion of what inflammatory changes look like in dark tone skin. Inclusive skin inspection is included in the EWMA ‘Wound curriculum for student nurses — European Qualification Framework Level 4’ but not in the Registered Nurse versions, these latter documents were developed between 2017–20. It would be good practice to review and update these guidelines to reflect inclusive skin inspection guidance.
A second survey will be run to assess the impact that this has on staff confidence with different skin tones once 85% of the staff have received the new training that is specific to pressure damage and darker skin tones.