The importance of promoting wound healing through the selection of appropriate compression bandages and dressings, while also considering the individual needs of patients, particularly those marginalised in society (e.g. people experiencing homelessness), was emphasised. The symposium concluded with the presentation of several case studies that highlighted various aspects of venous leg ulcer (VLU) care, exudate management (leakage avoidance) and patient perspectives.
Living with a leg ulcer
The symposium began with an emotional video featuring patients describing the physical, emotional and social impacts of living with a leg ulcer. Many patients spoke of pain unlike anything they had ever experienced. One patient, overwhelmed by the pain, admitted to asking for their leg to be amputated. Another, who had lived with a leg ulcer for three years, described the experience as feeling like “hell.”
Wound leakage was another significant issue for many individuals. One woman shared that she has to have her dressing changed three times a week to manage the constant leakage, which not only prevents her from attending social events but also stops her from exercising, as she fears that any physical activity could lead to complications and delay her healing process, leaving her feeling as though she is “back to square one.”
Another woman described how she had to make adjustments at home to cope with her wound leakage. She now covers her furniture with plastic sheets or bin bags to prevent stains from the exudate. To prepare for the seepage, she keeps spare clothes and socks close by, as the exudate often soaks through her bandages and begins to smell, leaving her feeling embarrassed. Her family life has also been significantly affected. She can no longer do housework or participate in activities with her grandchildren due to the constant pain and now relies entirely on her husband for support, which makes her feel guilty.
One man expressed embarrassment at the thought of his family, friends or neighbours seeing or smelling his wound, which has led him to withdraw further from social situations. Instead, he relies on leg clubs not only for help with changing his dressings but also as his only source of social engagement. These clubs allow him to connect with fellow leg ulcer patients in a space where he can feel understood, without the fear of embarrassment or shame.
Patients with VLUs often experience the following (Hellström et al, 2016; Stechmiller et al, 2019; Folguera-Álvarez et al, 2022):
- Poor quality of life
- Low self-esteem
- Sleep disruption and fatigue
- Chronic pain
- Functional reduction and behavioural adaptations
- Social isolation
- Anxiety and depression.
Wound leakage causes (World Union of Wound Healing Societies [WUWHS], 2019):
- Discomfort
- Increased frequency of dressing changes
- Increased pain
- Behavioural adaptations
- Damage to clothes, bedsheets and soft furnishings in the home.
Sarah Gardner then took the audience through the epidemiological data related to VLUs, including patient profiles, risk factors and socioeconomic factors. She also detailed the costs associated with VLU treatment to the United Kingdom’s National Health Service
VLUs are the most common type of leg ulcer, accounting for 60–80% of cases. They affect approximately 0.1–0.3% of the population, with their incidence increasing with age. The lifetime risk of developing a VLU is about 1%, and these ulcers occur across all socioeconomic groups. However, it is important to note that poor healing and higher recurrence rates are often observed in individuals from lower socioeconomic backgrounds (Nelzén and Frannson, 2007; National Institute for Health and Care Excellence (NICE), 2024, Sen, 2019).
The economic burden of VLUs on the NHS is significant, with annual costs estimated to be between £500 million and £900 million. On average, the cost of wound care for a single VLU is approximately £7,600 per year. Furthermore, the annual cost associated with a non-healing VLU can reach £13,500, in stark contrast to just £300 for a healed VLU.
Pathophysiology of VLUs
Venous hypertension is a result of chronic venous insufficiency, which is secondary to problems with valve incompetence and an impaired calf pump muscle (Wounds UK, 2022; NICE, 2024). These factors result in increased pressure in the venous system, which subsequently increases the permeability of the capillary walls. This causes oedema, leakage of red blood cells and leukocyte infiltration and activation (Mansilha and Sousa, 2018). Patients may experience skin alterations and deterioration of the skin and subcutaneous tissue, leading to high levels of exudate and, ultimately, ulceration.
Non-healing VLUs remain stuck in the inflammatory phase, producing high levels of exudate. Elevated inflammatory mediators and proteolytic enzymes in the exudate break down and disrupt the formation of new extracellular matrix. The exudate in these non-healing wounds is more toxic and harmful than healing wounds, leading to further skin breakdown as the wound increases in size (Gardner, 2016). Sarah made the point that these high levels of exudate have become ‘normalised’ within the medical system.
Terminology of VLUs
The terminology used to describe the condition, such as ‘wet leg’ or ‘leaky leg,’ is problematic as it does not constitute a diagnosis and may perpetuate the perception that high levels of exudate are ‘normal.’ These terms should not be written or documented in patients’ notes, as they reflect the consequences of unmanaged venous disease and unhealed wounds rather than a diagnosis. Sarah argued that language is key and called for a change in terminology when referring to these types of wounds.
Sarah then examined the aetiology of VLUs and highlighted six key areas that impact the quality of life of individuals suffering from the condition [Table 1].
Quality of life
Sub-optimally managed wounds and exudate leads to a cascade of physical, psychological and social problems, although these issues are often not routinely acknowledged, documented or addressed by clinicians. The authors note that, anecdotally, a cancer diagnosis often elicits support and understanding from friends and family, whereas VLUs tend to lead to feelings of shame, disgust, and isolation. This disparity highlights how the stigma surrounding VLUs can exacerbate the emotional and social burdens on patients, further complicating their recovery and quality of life. To further explore the impact of exudate on patients with VLUs, refer to Sarah’s article in The Community Nursing Journal (Gardner, 2024).
Odema: ‘The root of many evils’
Dot Weir took the stage and addressed the challenges associated with oedema, describing it as the “root of many evils.” While complications of oedema are well-documented in patients with hard-to-heal VLUs and lymphoedema, other forms of oedema, such as dependent oedema in wheelchair users and patients with limited mobility or impaired blood supply to the calf muscle, are often overlooked.
When there is a challenge with oedema, there is also a challenge with perfusion. In healthy tissue, oxygen can diffuse easily through capillaries. However, when tissue is filled with fluid, capillaries are spread apart, increasing the distance for oxygen diffusion (Scallan et al, 2010; Ince, 2015; Saravi et al, 2023). Therefore, there are numerous reasons to address oedema, not only in patients with venous disease but in various other clinical scenarios.
What is the right intervention?
Dot posed the question, “When is it best to intervene?” For instance, understanding the presence of underlying conditions such as congestive heart failure is important. She noted that patients with plantar diabetes-related foot ulcers are often advised to limit mobility, which can exacerbate oedema and impair the healing process.
We know that compression therapy is considered the ‘gold standard’ treatment for VLUs. Research reports that compression therapy doubles the chances of a VLU healing (O’Meara et al, 2012; Nelson and Adderley, 2016). Dot went on to acknowledge the importance of assessing blood flow to the limb/foot to determine the appropriate level of compression. She also discussed the limitations of diuretics for managing oedema, explaining that while diuretics can be beneficial for oedema related to cardiovascular issues, they are not ideal for general oedema management as they can dehydrate the patient (Arumugham and Shahin, 2023). When used on the right patient in the right way, compression therapy is the best treatment to improve venous return, reduce oedema, heal VLUs and improve the skin, thereby reducing the risk of recurrence. The earlier that compression therapy can be started, the better the outcome is likely to be (National Wound Care Strategy Programme, 2020).
Compression therapy options include:
- Multilayer wraps
- Compression stockings and socks
- Juxtaposed strap garments
- Compression pumps
- Elastic tubular bandages for oedema management
- Oedema Wear Fuzzy Walle Stockinette
- Reusable lightweight compression wraps.
How do we encourage engagement with compression?
As compression is a long-term treatment, individuals must be motivated and engaged in their own care (Wounds UK, 2021). Education is key to encouraging patient engagement and acceptance of compression therapy. Patients need to understand that venous insuffciency is a lifelong condition and that compression therapy will always be needed. This need continues even after a wound has closed, as closure does not necessarily indicate complete healing.
The choice of compression should be based on individual assessment and tailored to the patient’s lifestyle, ensuring it is as comfortable and pain-free as possible (Wounds UK, 2022). A holistic assessment should evaluate vascular status, limb shape and size, oedema, ulcer size, and the patient’s capability and willingness to participate in their care (Wounds International, 2022). Additionally, patients should feel a sense of agency over their compression pathway. Factors such as workplace and environmental considerations, comfort, appearance and drainage must be addressed alongside practical aspects of wound care.
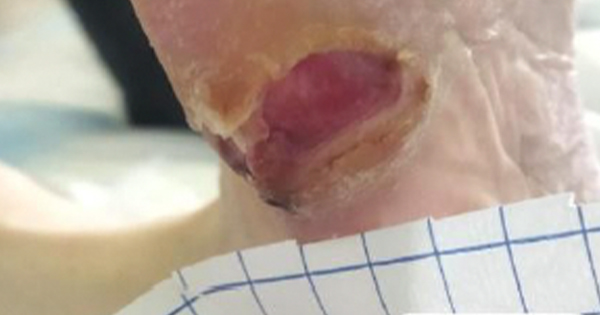
Providing patients with comprehensive information about their treatment regimen is important. Dot gave an example of a patient who had not been informed that compression stockings should be removed periodically. After three weeks of continuous use, the patient developed bilateral wounds from the stocking’s interior cutting into the anterior part of the ankle [Figure 1]. Consequently, the treatment regimen was adjusted to include limb and wound hygiene, which led to an improvement in the patient’s dermatitis within three weeks. The patient was then informed that compression wraps should also be removed periodically.
A study by Perry et al (2022) found that the provision of compression is challenging due to organisational barriers, including heavy workloads, lack of knowledge, insufficient training and prescribing issues. Patient engagement barriers have also been identified, with some patients finding compression uncomfortable or difficult to wear, particularly in hot weather (Perry et al, 2022; Lian et al, 2023).
A holistic approach is necessary to address these barriers. For instance, clinicians should acknowledge that expecting patients to quit work is often unrealistic, as it would significantly impact their quality of life. Furthermore, certain wounds, such as those located posterior to the malleoli bone, are particularly hard to dress. Compression wraps may “hammock” over this area, which is often tender, requiring comfort measures like foam padding to reduce discomfort and enhance oedema management.
Additionally, elderly patients may face difficulties with compression therapy due to decreased dexterity, either personally or through their carers. As such, patient goals should be revised and managed collaboratively to help improve patient engagement and engagement to compression therapy.
Case studies
Dot went on to show three case studies where appropriate dressing choices greatly impacted healing and the quality of life of patients.
Case study 1
A 70-year-old man with type 2 diabetes, chronic kidney disease, venous insufficiency and Crohn’s disease presented with significant oedema and ulceration on his left anterior lower extremity. The VLU was heavily exudating [Figure 2a].
Initial management included the application of a four-layer compression wrap in conjunction with Mepilex® Border Flex (soft silicone-coated multilayer foam dressing). Within five days, oedema measurements showed improvement: the foot circumference decreased from 33cm to 25.5cm, the ankle from 39cm to 30.5cm, and the calf from 55.5cm to 54cm [Figure 2b–c]. By sharing the progress of the measurements with the patient, there was increased understanding and greater engagement with compression. The plan of care was continued [see Figure 2d for day 23 of treatment], leading to subsequent healing of the wound.
Case study 2
A 56-year-old male construction worker with a history of multiple VLUs presented with a VLU measuring 4cm (length) x 4cm (width) x 1cm (depth), with a 1.2cm undermining in the 6—12 o’clock region [Figure 3a]. He had no other significant health issues. The wound was initially managed with a gelling fibre (primary) dressing, Mepilex® Border Flex (secondary) dressing and a four-layer compression wrap. However, under the gelling fibre dressing, exudate continued to pool.
The patient and wound were subsequently reevaluated to discuss an alternative treatment regimen. Following this reevaluation, the primary dressing was changed to Exufiber® Ag+ (silver-containing gelling fibre dressing), while Mepilex® Border Flex and the four-layer compression wrap were continued. This adjustment resulted in an improvement in healing and by day 23, healthy granulation tissue was observed [Figure 3b]. After 40 days of treatment, the Exufiber® Ag+ dressing was discontinued [Figure 3c], and by day 67, the wound had achieved complete closure [Figure 3d].
Case study 3
A 69-year-old male active retired corrections officer presented with numerous small ulcers on his leg surrounded by eroded tissue [Figure 4a]. His medical history included chronic venous insufficiency. He had been using 100 abdominal gauze pads per month and self-treating with a zinc barrier over the entire lower leg, along with wrapping from ankle to knee with Unna’s boot. His dressings were changed daily, and he was initially insistent that he could not tolerate compression therapy.
The patient was first informed about cleaning the wound and compression procedures to ensure he felt in control of his care. His leg was first cleaned of eroded tissue, and Exufiber® Ag+ was applied along with a large super-absorbent dressing. Within three days, there was a dramatic improvement [Figure 4b]. Treatment continued with a twice-weekly two-layer wrap that was comfortable for the patient. By ten weeks, the wound was fully closed [Figure 4c].
Building patient trust and a sense of control were important to support the patient through compression therapy to wound closure. Having a variety of dressings and combinations of dressings available in one’s toolbox helps improve the quality of life for patients and their families during a stressful time.
Exudate management – hidden stigma and quality of life
Jemell Geraghty drew the symposium to a close with a presentation about her experience of exudate management working with people experiencing homelessness in London. Language is key when talking about people experiencing homelessness, as many negative labels and stigma are associated with homelessness. However, Jemell drew attention to the fact that language is changing to be more person focused. For example, ‘IDU’ (injecting drug users) is no longer used and is being replaced with ‘people who inject drugs’, and ‘homeless’ is now ‘people who experience homelessness’. This shift in language reflects a move towards greater respect and understanding of the individual.
Within the community, three categories are identified (Malik and Geraghty, 2021):
People actively injecting
- Injecting into the lower limb (groin, foot, toes) and living with lower limb ulcers or associated wound and/or skin conditions.
People who have ceased injecting
- Still at risk of living with a wound and/or lower limb/foot condition.
People who have never injected (often missed in literature)
- Lower limb or foot wound as a result of other factors (medical/family/lifestyle)
- Multiple pregnancies and deep vein thrombosis can cause excessive oedema and ulceration
- At risk of developing lower limb or foot wound and/skin condition
- Often stigmatised as drug users because of their homelessness.
Jemell provided an example, based on her recent PhD studies, “exploring the experiences of injecting drug users living with leg ulceration” (Geraghty and Kendall, 2021), of a young woman who, despite a history of injecting drug use, was diligently managing her leg ulcer. She maintained a diary detailing the pain, the impact of the leakage and her careful cleaning of the wound. The findings of this study challenge the myth and stereotype that people experiencing addiction, chaotic lifestyles or homelessness do not care about their wounds or their healing. There is a need to understand this group of people and help work with the individual to identify their priorities and develop a shared plan of care.
Jemell then discussed the concept of enacted stigma, drawing on Erving Goffman’s work on stigma. It is important to look beyond the wound and at the stigma the person may experience because of their lifestyle. For example, a poor consultation with a clinician or negative reactions from someone in the clinic can impact their attitude towards caring for their wound and engagement with treatment.
Conclusion
Inappropriate dressings applied by clinicians that overlook an individual’s lifestyle can lead to poor exudate management and engagement with treatment. On occasion, the patient can be blamed, when there are many factors to consider, including the choice of the clinician. Jemell explained that taking the time to talk to the patient and understand their story, choose the right dressing and properly wash the skin is like ‘the magic wand,’ transforming not only the wound but also the individual.
Access to effective healing and exudate management should be available to everyone, not just those in mainstream society. A supportive and understanding clinical environment can promote patient engagement, improve healing rates and enhance quality of life.