Wound healing is a complex physiological process the aim of which is to re-establish homoeostasis following epidermal surface damage. The phases required for wound healing include inflammation, re-epithelisation and scar formation (Shaw and Martin, 2009). Immediately after tissue damage, an inflammation process is triggered and polymorphonucleocytes and monocytes migrate to the damaged cutaneous tissue.
The main role of these immune cells in wound healing are to remove cell debris, and devitalised tissue and bacteria with the aid of released metalloproteinases (MMPs; Krejner and Grzela, 2015). While acute wounds heal in days or weeks, chronic wounds require longer periods of time or fail to heal entirely, mainly due to excessive degradation of extracellular matrix (ECM), an indication of imbalanced MMP, human neutrophil elastase (HNE) and human calprotectin (HCP) levels and their inhibitors (Krejner and Grzela, 2015).
MMPs are a family of zinc-dependent proteinases and along with their inhibitors, play an essential and beneficial role in all normal wound healing phases (Power et al, 2017). These proteinases aid ECM removal and migration of immune cells to the injured tissue in addition to being mediators of reepithelialisation (Cabral-Pacheco et al, 2020). Under normal conditions, MMP levels rapidly increase during the first days following damage, subsequently followed by a decrease after day five. Elevated MMP concentrations have been reported in chronic wounds (Krishnaswamy et al, 2017). Increased levels in wound exudate have been shown to correlate with poor wound healing (Sabino et al, 2015).
Human neutrophil elastase (HNE) is a serine elastase which can be present at a high concentration during wound healing (Ferreira et al, 2017). Neutrophil-mediated inflammation, as observed in acute wounds, leads to the local release of HNE (Fujishima et al, 1995). Typically, proteinase inhibitors protect epithelial cells from proteolysis by HNE (Henriksen and Sallenave 2008). However, high HNE concentrations can contribute to extracellular matrix degradation.
In a similar manner to HNE, human calprotectin (HCP) is a cytosolic protein that is expressed in neutrophils and induced during inflammation (Hu et al, 1996). Human calprotectin plays a role in the expression of pro-inflammatory cytokines such as IL-1B, TNF-a and IL-6 (Jukic et al, 2021). If homoeostasis during inflammation is not maintained, HCP can contribute to further inflammation (Schonthaler et al, 2013).
Strategies to minimise excessive protease activity in chronic wounds include treatment of the underlying cause, wound bed preparation and the patient’s general status (Kolahreez et al, 2024). Products have been developed that modulate and/or absorb excess biomolecules such as MMPs, human neutrophil elastase and human calprotectin (Krejner and Grzela, 2015; Veličković et al, 2020). Foam-based wound dressings have also been developed that absorb elevated levels of exudate production and have increased absorbance levels when compared to traditional cotton wool- and lint-based dressings (Gefen et al, 2023). While certain foam dressings have relatively high levels of fluid absorption, limited scope in mode of action results in restricted applications options.
Recently developed dressings containing superabsorbent polymer (SAP) have demonstrated improved absorption capacity over conventional foam-based dressings (Veličković et al, 2022; Cutting and Westgate, 2023). Further advances in SAP dressings have included a silicone contact layer to avoid damage of the surrounding skin and minimise patient pain during dressing changes (Barrett et al, 2020). The removal of protein exudate and protection of the patient’s wound contributes towards more effective wound healing (Power et al, 2017).
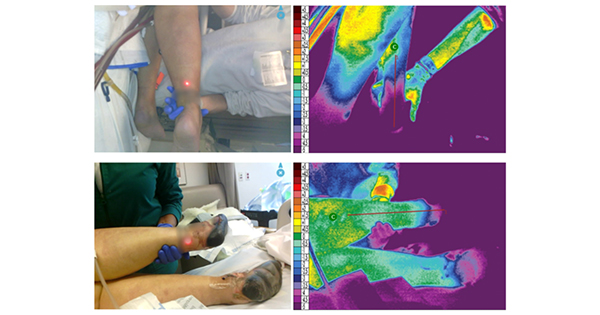
In this study, a self-adhesive SAP silicone dressing, Zetuvit® Plus Silicone Border (also known as RespoSorb® Silicone Border, Paul Hartmann AG) was evaluated for its ability to modulate MMPs, human neutrophil elastase and human calprotectin. Results were compared to six silicone foam dressings, with some containing a lock-away SAP layer, and one wound contact layer-only.
Ethical approval
No ethical approval was required for this study.
Methods
Test dressings
A total of eight wound dressings were included for analysis:
- Zetuvit® Plus Silicone Border (Paul Hartmann AG; self-adhesive silicone SAP dressing).
- ALLEVYN® Life (Smith+Nephew; silicone foam dressing 1).
- Mepilex® Border Flex (Molnlycke; silicone foam dressing 2).
- Biatain® Silicone (Coloplast; silicone foam dressing 3).
- ALLEVYN® Gentle Border (Smith+Nephew; silicone foam dressing 4).
- Aquacel® Foam (Convatec; silicone foam dressing 5).
- Aquacel® Foam Pro (Convatec; silicone foam dressing 6).
- N A™ Knitted Viscose (non-silicone wound contact layer-only).
Modulation of MMP activity
Eight test dressings (self-adhesive silicone SAP dressing, silicone foam dressings 1–6 and wound contact layer-only) were cut aseptically into 1.0 × 1.0 cm sized samples in triplicate, placed into a 24-well plates (Falcon; Corning, UK) and activated with 1 ml of deionised water. Control wells were prepared with deionised water only. Working solutions of recombinant human MMP-2 and MMP-9 (Abcam, UK) were prepared to 5 ng/ml according to manufacturer’s instructions and a 250 µl aliquot of each proteinase was added to their respective dressing and control wells. Plates were incubated at 37 ± 2°C and 50 ± 5 rpm for 24 hours. After incubation, dressing samples were removed and 1 ml of sterile phosphate buffered saline (Scientific Laboratory Supplies) was added to each well. Plates were further incubated on a shaking platform (50 ± 5 rpm) for 1 hour at 37 ± 2°C, then supernatants were collected and vortexed. The quantity of recovered MMP 2 and MMP-9 for each dressing was analysed using the Human MMP2 SimpleStep ELISA® kit and the Human MMP9 SimpleStep ELISA® kit (Abcam, Cambridge, UK) respectively, according to manufacturer’s instructions.
Optical densities were measured at 450 nm and 550 nm for MMP-2 and 450 nm and 570 nm for MMP-9. Standard concentration curves of each MMP-2 and MMP-9 at the appropriate wavelengths were also performed and data plotted according to manufacturer’s instructions. Optical densities were normalised against background detection and compared to the respective standard curve to obtain a final protein concentration.
Modulation of human neutrophil elastase and human calprotectin activity
Eight test dressings (self-adhesive silicone SAP dressing, silicone foam dressings 1–6 and wound contact layer-only) were prepared in the same manner as the MMP assay. Working solutions of recombinant human neutrophil elastase (HNE) (10,000 pg/ml) and human calprotectin (7,000 pg/ml) were prepared and a 250 µl aliquot of each protein was added to their respective dressing and control wells. Plates were incubated and recovered according to the same process as the MMP assay.
For each individual sample, 100 µl was analysed in duplicate using either the Human Neutrophil Elastase ELISA Kit (Abcam, UK) or the Human Calprotectin ELISA kit (Abcam, UK). Optical densities were measured at 450 nm and 550 nm and processed as described for the MMP assay.
Statistical analysis
Data were tested for normality prior to individual comparisons using the Shapiro–Wilk analysis. Comparisons of the mean between dressing types was conducted with a two-sample Student’s t test. Data were considered significant at p<0.05, p<0.01 or p<0.001.
Results
Modulation of protein sequestration
MMP sequestration
Following 24 hours incubation with self-adhesive silicone SAP dressing, a 100% reduction in MMP-2 and MMP-9 was observed (p<0.001) when compared to the wound contact layer. All remaining test dressings demonstrated <48.1% reduction in MMP-2. When tested for MMP-9, three silicone foam dressings showed >90% reduction in MMP-9 (dressing 2 = 92.00%, dressing 3 = 93.25% and dressing 5 = 92.78%) compared to the wound contact layer only dressing, whereas the remaining silicone foam dressings (dressings 1, 4 and 6) demonstrated between 38.5% and 47.8% reduction [Table 1 and Figure 1].
Human neutrophil elastase sequestration
Following 24 hours incubation with self-adhesive silicone SAP dressing, a significant >99.99% reduction in HNE was observed (p<0.001) when compared to the wound contact layer [Table 1 and Figure 2]. Silicone foam dressings 3, 5 and 6 demonstrated a significant >98% reduction, whereas silicone foam dressings 2 and 4 had a reduction >64%. No reduction in HNE concentration was identified for silicone foam dressing 1.
Human calprotectin sequestration
Following 24 hours incubation with self-adhesive silicone SAP dressing, a significant 85.43% reduction in human calprotectin was observed (p<0.001) when compared to the wound contact layer [Table 1 and Figure 3]. Silicone foam dressings 1 and 3 demonstrated <74% reduction in human calprotectin. No reduction in human calprotectin concentration was identified for silicone foam dressings 2, 4, 5 or 6.
Discussion
Wound healing is a complex process initiated following a cutaneous injury. Several wound dressings with differing compositions have been developed to treat wounds. An optimal wound dressing maintains wound moisture, manages excess exudate and proteinases and prevents or controls infection (Lin et al, 2016). Exudate production aids wound healing by maintaining wound bed moisture, mobilising tissue repair cells and removing devitalised tissue. Excessive exudate can delay the healing process, partially due to unbalanced levels of MMPs and their inhibitors (Brown, 2017; Kandhwal et al, 2022). Periwound skin maceration, leakage, malodour, pain, discomfort and higher risk of infections are problems related to elevated levels of exudate, typically observed with chronic wounds (Brown, 2017). Managing excess exudate is therefore a critical process during wound treatment and poses a challenging factor in clinical practice. This study presented a comparison of dressing capabilities for modulation of several different proteins important during wound healing.
MMPs are responsible for initiating the breakdown of damaged cutaneous tissue during wound healing. While the presence of these proteinases produced by immune cells is essential to trigger the healing process, their activity tend to be downregulated by issue inhibitors in the later phases of wound healing. In hard-to-heal wounds, abnormal ratios of MMP/inhibitor are usually detected, suggesting a negative role of MMPs in the final stages of wound healing (Barrett et al, 2020). This includes chronic wounds such as diabetic foot ulcers (Liu et al, 2009; Muller et al, 2008).
In the current study, of the eight wound dressings examined for MMP-2 and MMP-9 modulating capabilities, only the self-adhesive silicone SAP dressing was capable of total reduction of both proteinases. This finding suggests that the self-adhesive silicone SAP dressing is an improved candidate for treatment of hard-to-heal chronic wounds when compared to the foam-based wound dressings.
HNE functions as an enzymatic protease and antimicrobial, which is stored in azurophilic granules and are exocytosed at a later stage compared to other proteases such as MMPs (Wilgus et al, 2013). Extracellular matrix degradation assists neutrophil extravasation during inflammation (Watanabe et al, 1990). However, high concentrations have been identified in chronic wounds (Vogl et al, 2004), and increased protease activity can increase epithelial damage (Wilgus et al, 2013). The SAP dressing was observed to sequester a significantly greater concentration of HNE compared to the majority (4/6) of the foam-based dressings, with an average of 0.07 pg/ml remaining in the plate following the absorption period.
HCP plays an important role in the modulation of the inflammatory process and recruits several biomolecules (such as leukocytes) to the source of inflammation during early wound healing (Vogl et al, 2004). The presence of HCP also contributes to neutrophil chemotaxis (Jukic et al, 2021). However, if not controlled, excessive HCP can cause a deleterious effect on inflamed tissues (Yui et al, 2003).
In the current study, SAP dressings were demonstrated to sequester a greater concentration of HCP than all foam-based dressings, with a significantly greater concentration than 3/6 of those dressings. Enhancing exudate removal at a wound location prevents negative implications of HCP if inflammation is prolonged, maintaining the routine healing process.
Wounds with moderate to elevated levels of exudate are treated primarily by SAP dressings, with foam, alginate, hydrofiber and hydropolymer based dressings recommended as the second line for wound management (Velickovic et al, 2023), in line with the greater absorption efficacies of superabsorbent dressings witnessed over foam-based dressings (Cutting and Westgate, 2012; Veličković et al, 2022). Dressings with elevated absorbency properties minimise the frequency of dressing changes during a wound treatment course, with a direct impact on time and cost savings, as well as the patient’s quality of life (Barrett et al, 2020). SAP dressings have shown improved wound healing processes when managing wounds with moderate to elevated exudate levels, with reduced damage to the periwound skin and, consequently, lower pain levels in the patient (Barrett et al, 2020).
Structural differences between the dressing types may contribute to the differences observed in protein exudate levels. As part of the SAP dressing mode of action, the layers are designed to lock fluids into the retention layer away from the wound. This may have contributed to an increased retention when compared to the foam-based dressings.
Conclusion
The self-adhesive silicone SAP dressing showed to be a more effective choice of dressing for conditions simulating wounds with healing impairment and/or elevated wound healing inhibitors. The self-adhesive silicone SAP dressing successfully modulates excess proteinases when compared to similar foam-based dressings, reducing the chances of contamination and the need of frequent dressing changes. Taking into consideration the various aspects of wound dressings, this in vitro study has shown that the self-adhesive silicone SAP dressing potentially provides a series of positive benefits for patients during wound treatment. Further investigations on the real benefits of the self adhesive silicone SAP dressing from real clinical scenarios are needed.