Over the past two decades, Sweden has significantly advanced lymphoedema treatment, moving from traditional passive methods to proactive approaches involving exercise, self-care and early diagnosis. Initially, research demonstrated that physical activity, even heavy weightlifting, does not worsen lymphoedema, challenging previous assumptions. This shift supported increased physical activity among patients, leading to improved outcomes.
Key developments include establishing thresholds for diagnosing mild lymphoedema. Additionally, new methods measuring local tissue water, like the Finnish Lymphscanner, have enhanced early diagnosis in both upper and lower limbs, enabling timely interventions and potential regression of mild lymphoedema.
The implementation of surveillance programmes utilising tools such as the Lymphedema Quality of Life Inventory (LyQLI) has facilitated the management of problems related to the chronic condition.
Within surgery, research has focused on the pathological role of adipose tissue in chronic lymphoedema. Initially met with scepticism, pioneering work demonstrated that adipose hypertrophy, driven by inflammation, contributes significantly to limb swelling. Using advanced imaging and molecular analyses, it was established that liposuction effectively reduces adipose tissue and limb volume and decreases complication rates, such as erysipelas. Collaboration with international centres facilitated training and implementation of liposuction worldwide.
Swedish guidelines now emphasise active treatment, including exercise and compression, moving away from passive therapies like manual lymph drainage. Efforts to adapt measurement techniques for lower limbs have improved early detection there too. Education and dissemination of knowledge are supported by networks within the Swedish Society of Lymphology and collaborations through national centres, seminars and international congresses.
Despite regional disparities, the creation of consensus recommendations and development of specialised centres aim to standardise care. Academic institutions, such as Lund University and Karolinska Institutet, provide specialised training, though there’s a need for broader physician education. Overall, these advancements reflect a positive trajectory, promising continued improvements in lymphoedema management in Sweden.
Karin Johansson
The earliest Swedish publication in the Journal of Lymphoedema (JoL), dating back to 2007, resulted from my collaboration with Professor Neil Piller at Flinders University in Adelaide, Australia (Johansson and Piller, 2007). It focused on exercise for patients with lymphoedema. Conducted in 2004, this study addressed a then-controversial question: could breast cancer-related arm lymphoedema patients safely engage in exercise without risking deterioration?
This concern gained renewed significance around the year 2000, when evidence showed that increased physical activity improved survival rates among breast cancer patients. However, this raised questions about whether patients with lymphoedema should limit their activity, potentially reducing their chances of survival compared to patients without lymphoedema who could exercise freely. Interestingly, my 2002 dissertation, based on a case-control study, found that breast cancer patients in the 1990s who continued their normal activities — including exercise — had a lower incidence of lymphoedema than those who strictly followed restrictive recommendations (Johansson et al, 2002).
Following the Australian exercise study, several further studies emerged both in Sweden (Lindquist et al, 2015) and internationally, including collaborations with Professor Kathryn Schmitz at the University of Pennsylvania, Professor Sandi Hayes at Griffith University in Australia. Today, we know that even heavy weightlifting can be safely performed without worsening lymphoedema.
Another significant paper published in JoL, by Stanton et al (2006), helped clarify diagnostic criteria for arm lymphoedema. They identified a threshold of approximately 5% in lymphoedema relative volume (LRV) for diagnosing mild arm lymphoedema, aligning with our clinical experience that had been developed over 10 years. Along with palpation of increased skin fold thickness and tissue tension, this threshold was adopted in surveillance programmes at the Lymphedema Unit at Skåne University Hospital in Lund. A 10-year follow-up revealed that 90% of the patients maintained low levels of lymphoedema (<20% LRV)(Johansson and Branje, 2010), leading to its inclusion in the Swedish National Lymphedema Guidelines.
This development illustrates the transition in Swedish lymphoedema care from treatments that passivise patients — such as manual lymphatic drainage (MLD) and restrictive “don’t do” lists — to active methods with an emphasis on exercise, self-care and compression garments. Furthermore, this shift in healthcare philosophy moved from reactive treatment to proactive prevention, including early diagnosis and intervention (Johansson et al, 2023). This transition called for a method to measure lymphoedema quality of life. And again, the solution was found in Australia in a disease specific questionnaire, developed at Edith Cowan University in Perth. The Lymphedema Quality of Life Inventory (LyQLI)(Klernäs et al, 2015) was adapted for Sweden and it has proven valuable for long-term evaluation and identifying later-stage problems.
Another research cooperation, this time with Professor Peter Mortimer at St George’s University in London, revealed evidence for lymphatic origin with thrombosis Axillary web syndrome (Johansson et al, 2020)
Research further explored early diagnosis in arm lymphoedema, incorporating measurements of local tissue water via devices like the Finnish Lymphscanner, introduced to Sweden in 2010. These methods enabled more reliable early detection and, importantly, demonstrated that mild lymphoedema could even regress with appropriate management.
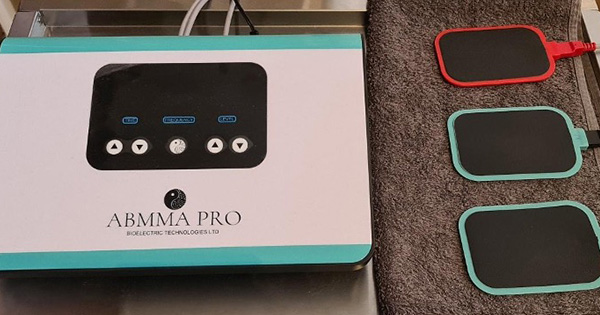
While most research in Sweden has focused on breast cancer-related arm lymphoedema, partly due to challenges in reliably measuring lower-limb lymphoedema, recent advances have addressed this gap. Testing various measurement techniques (Figure 1) on both healthy and affected individuals has allowed us to establish thresholds for lower-limb lymphoedema (Jönsson et al, 2022), facilitating earlier detection and treatment, with the goal of preventing progression similar to upper-limb cases.
Håkan Brorson
“Adipose tissue in lymphoedema? I have never seen it. Is that something peculiar to Swedes?” This remark was made by a senior figure in the field of lymphology following my presentation entitled ‘High Content of Adipose Tissue in Chronic Arm Lymphedema Limits Treatment Outcome’ at the 2000 National Lymphedema Network Conference in Orlando, Florida (Brorson, 1998; 2004).
During my first participation in the International Congress of Lymphology in Madrid in 1997, I presented several studies demonstrating the marked efficacy of liposuction in treating chronic, non-pitting postmastectomy arm lymphoedema. I specifically highlighted the significant presence of adipose tissue in these cases. This line of research was subsequently summarised in my doctoral dissertation in 1998.
Scepticism greeted my findings on liposuction for lymphoedema, with critics dismissing it as science fiction. Encouraged by Professor Witte, I explored cases showing persistent limb volume due to adipose tissue, confirmed by MRI. Early Swedish lymphangiography and unsuccessful procedures highlighted the challenges faced before liposuction proved effective.
The first liposuction procedure for lymphoedema was performed in 1987. However, it was not until 1993 that a comprehensive treatment protocol was developed. At the time, the concept of adipose tissue accumulation as a component of lymphoedema was largely unrecognised and met with suspicion. In light of this, and building upon the clinical observations described above, I was motivated to scientifically investigate and validate the pathological role of adipose tissue in lymphoedema that I had consistently observed in clinical practice.
Over the years, our research has consistently demonstrated — using computed tomography (CT) (Brorson et al, 2006), dual-energy X-ray absorptiometry (DXA), magnetic resonance imaging (MRI) (Hoffner et al, 2018), gas chromatography, as well as RNA sequencing, metabolomics and lipidomics analyses — that lymphoedema results not only in subcutaneous and intramuscular adipose tissue hypertrophy, primarily driven by local chronic inflammation, but also in muscular hypertrophy secondary to the mechanical load imposed by the increased limb weight. Following liposuction, both the pathological adipose accumulation and a significant portion of the muscle hypertrophy are reversed, leading to a complete reduction of excess limb volume.
An additional clinical benefit observed postoperatively is a substantial reduction in the incidence of erysipelas — by 87% following liposuction for arm lymphoedema, and by 65% in cases involving the leg.
Initial concerns were raised regarding the potential for liposuction to further damage lymphatic structures. However, lymphoscintigraphic studies have shown that liposuction does not result in any additional impairment of lymphatic transport capacity (Brorson et al, 1998).
Several peer-reviewed studies have demonstrated significant improvements in health-related quality of life following liposuction for lymphoedema.
To support global dissemination of the technique, we have hosted and trained 43 multidisciplinary teams from various countries through structured weekly visits to the Lymphedema Unit at the Department of Plastic and Reconstructive Surgery, Skåne University Hospital, Malmö, Sweden. These teams have successfully implemented the method within their respective national healthcare systems.
Our research has further benefited from international collaborations, notably with Professors John Boyages, Louise Koelmeyer, and Thomas Lam at the Australian Lymphoedema Education, Research and Treatment (ALERT) programme at Macquarie University Hospital, Sydney, Australia, and with Professors Arin Greene and Dhruv Singhal at the Boston Lymphatic Center, Harvard Medical School, Boston, USA.
Long-term follow-up studies have consistently shown that liposuction, when combined with controlled compression therapy, results in a complete and sustained reduction of excess limb volume, with no recurrence (Hoffner et al, 2018).
The Swedish National Board of Health and Welfare recognised and endorsed this treatment as early as 1998 for use in Malmö. In 2025, the board extended approval for the procedure to be performed at Karolinska University Hospital in Stockholm and Uppsala University Hospital in Uppsala. Both centres have received training from the Malmö team to ensure standardised implementation of the technique.
In general
The significant findings through the years have step by step been included in the National Guidelines for Cancer Rehabilitation but also in different guidelines for cancer treatment. Those guidelines always refer to the National Lymphedema Guidelines that are constantly updated.
But Sweden is a large country in terms of surface area and lymphoedema programmes that are suitable for densely populated areas may not work in less populated areas. However, through networks within National Cancer Centers and the Swedish Society of Lymphology (Svensk Förening för Lymfologi, SFL) information and education are spread to healthcare professionals through webinars and seminars. The focus is on new findings that can clarify certain processes and outcomes, and on implementation in care. Swedish researchers have actively taken part in international congresses presenting their own research but also brought back new knowledge to Sweden. Through the years also many famous researchers in lymphology and lymphoedema have been invited to lecture.
One example of clarifying processes are rehabilitation ‘pyramids’. This work engaged the members of SFL to create consensus recommendations to identify lymphoedema problems and suggest care interventions. The intention is to use the pyramids in communication with other healthcare providers and representatives of healthcare and education to facilitate decision-making. This communication is essential as the lymphoedema care is not equal in Sweden and different regions can have completely different rules, for example for compensation for compression garments. This has been noted by the government and data collection and discussion about appropriate improvements are now being conducted with professionals, patients and appropriate organisations.
Education is also mediated by two universities in Sweden, at Lund University and Karolinska Institutet. However, these courses are only for physiotherapists, occupational therapists and nurses. The courses focus on the treatment of lymphoedema. But special courses for doctors are needed as diagnosis of primary lymphoedema stays a problem. It is very gratifying that a centre for the diagnosis and treatment of both primary and secondary lymphoedema recently was established in Stockholm. However, a broader approach is needed and SFL has taken on to try to influence the medical educations to start up or increase specialist short courses in lymphology, maybe digital, within the educational programmes.
As a summary of these 20 years, we do feel that important improvements and positive changes has been made in Sweden and we look forward with confidence (Figure 2).