Wound exudate is produced as part of the body’s natural healing process and contains nutrients, growth factors, immune mediators and immune cells that are essential for tissue repair and infection control (World Union of Wound Healing Societies [WUWHS], 2019). Exudate creates a moist wound healing environment, which is crucial for the removal of non-viable tissue and migration of tissue-repairing cells across the wound bed (WUWHS, 2019). When a wound is healing naturally through the standard stages of healing, the amount of wound exudate is highest during the initial inflammatory phase and gradually diminishes as healing progresses (WUWHS, 2019).
When the healing process is disrupted and a wound becomes chronic, excessive amounts of exudate may be produced (e.g. due to infection, prolonged inflammation, or underlying disease processes) and the exudate composition may change (e.g. elevated levels of inflammatory mediators and matrix-metalloproteinases prolonging the inflammatory phase of wound healing). If excessive and not managed effectively, exudate can lead to periwound maceration, delayed wound healing and an increased risk of infection. Moreover, it negatively affects patients’ quality of life (e.g. due to frequent dressing changes, leakage from dressings and malodour; WUWHS, 2019).
Besides treatment of the underlying conditions that contribute to excessive exudate (e.g. infection), effective management of exudate is crucial in wound care to ensure timely wound healing without complications (WUWHS, 2019). This involves the use of appropriate dressings that absorb and retain excess fluid, while maintaining a moist environment within the wound bed.
Gelling fiber dressings (also called hydrofiber dressings) are absorbent wound dressings that provide an ideal option for clinicians managing wounds with moderate to high levels of exudate. Gelling fiber dressings trap wound exudate within the structure of the matrix and subsequently form a soft gel, providing a moist environment to support the wound healing process. Other advantages include conformability to the wound bed, vertical wicking of exudate helping to reduce maceration, non-traumatic interaction with the wound and facilitation of autolytic debridement (Weller et al, 2020). This article examines the clinical performance and safety of Cutimed® Gelling Fiber in clinical practice.
Methods
A prospective observational study involving 36 patients was conducted in a German hospital from March 2022 to July 2023. The primary objective was to explore the absorption performance of the gelling fiber dressing and ability to prevent exudate accumulation in the wound (exudate management); secondary objectives included: condition of the wound margin; exudate level; wound area reduction; wound pain reduction; ease of use; comfort and satisfaction and safety parameters (i.e. any reported adverse events related to the gelling fiber, such as any disintegration of the dressing). See Box 1 for inclusion criteria and Box 2 for exclusion criteria. Patients presenting with a wound who met the criteria for treatment with the gelling fiber dressing were treated for 4 weeks with weekly assessments. Weekly assessments included:
- Documentation of wound-related parameters, e.g. wound size via photographic documentation software (tissue analytics); exudate level; condition of wound margins and periwound skin; signs of infection and wound pain (using the visual analogue scale [VAS])
- Documentation of product performance (exudate management) and safety parameters
- Documentation of dressing application and removal characteristics
- Patients’ and clinicians’ opinion.
- The last observation carried forward method was used to impute missing values when comparing variables between the start and end of the study.
Results
Patient and wound characteristics
A total of 36 patients were enrolled in the study. One patient was excluded at visit 3 due to a required change in treatment following a serious adverse event (not related to the study device or study itself). One patient presented with a healed wound (an expected outcome) at visit 3 and prematurely left the study but qualified for final analyses. The study analysis set therefore reflects data from 35 patients.
The mean age of the patients was 60.6 years (range: 23—82 years), with a male-to-female ratio of 68.6%/31.4%. Various concomitant conditions were present in the study population (e.g. diabetes mellitus, obesity). Of the wounds, 37% were diabetic ulcers, 9% leg ulcers, 34% surgical wounds, 6% traumatic wounds and 14% other (postoperative wound healing disturbances and a pressure ulcer caused by Hallux valgus). The low- to high-exuding wounds had been present for an average of 8.3 weeks and were covered with 0–42% slough (with >20% in 3 wounds) and 0–59% necrotic tissue (with >20% in 3 wounds) at the start of the study. Wound characteristics for all wound types can be found in Table 1.
The need for additional dressing changes between scheduled visits every 7 ± 2 days declined from 80% of patients at the start of the study to 57% by its conclusion.
Primary outcome
Exudate management
Effective exudate management is vital for timely wound healing without complications. Successful exudate absorption was documented by clinicians in 99.3% of all evaluations (n=138) and 100% of evaluations where compression therapy (compression class I or II) was used (n=18).
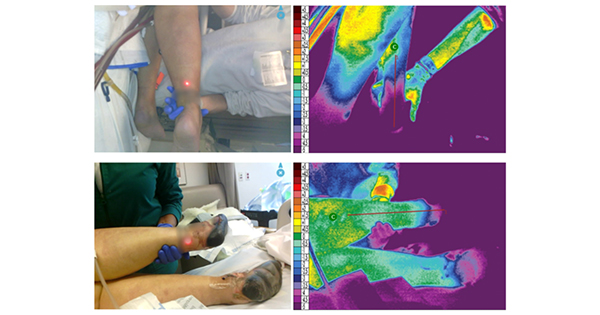
The amount of exudate remaining in the wound [Figure 1] was also documented by the clinician as ‘none’, ‘little’, ‘moderate’ or ‘much’. Little or no exudate was present in the wound in 98.6% of all evaluations, and in 94.4% of cases where compression was applied. Exudate was successfully transferred from the gelling fiber dressing to a secondary dressing in over half of the evaluations (64.2% of all evaluations; 55.5% with compression). Secondary dressings and additional wound care products included: gauze (16.2%), absorbent dressing (96.0%), hydrocolloid (1.7%), film dressing (15.0%), hydrogel (34.1%) and other products such as Cavillon lolly (6.9%), maceration protection (1.7%), skin care (0.6%) and sterile plaster (0.6%).
Secondary outcomes
Condition of the wound margins
Since poor exudate management can result in maceration, the state of the wound margins, periwound and surrounding skin is a crucial indicator of how effectively exudate is being managed. During the 4-week study period, the condition of the wound margins improved [Figure 2], indicating the exudate management efficacy of the gelling fiber dressing.
The percentage of patients with intact wound margins increased significantly from 25.7% at the start of the study (visit 1 [V1]) to 65.7% at the end of the study (visit 5 [V5]). The number of wound margins that were macerated decreased from 31.4% at V1 to 14.3% at V5, while those that were reddened decreased from 54.3% at V1 to 31.4% at V5. A slight improvement was also seen in the periwound skin (‘intact’ for 31.4% at V1/40.0% at V5; ‘macerated’ for 2.9% at V1/0% at V5).
Exudate level
As the wound progresses towards healing, the exudate level typically decreases. At the end of the study period, decreased exudate levels were observed for all wound types [Figure 3], indicating healing progress.
Wound area reduction
Reduction in wound area is often used as an indicator of wound healing progress. A substantial mean wound area reduction was observed across all included wound types* [Figure 4a].
The mean wound size significantly reduced from 6.7cm2 to 3.5cm2 (p<0.001), with a mean individual wound size reduction of 55%. Nineteen patients (55.9%) presented with a size reduction of at least 50% within the 4-week study [Figure 4b].
Three wounds healed completely during the study: a 4-week-old traumatic wound, a 20-week-old leg ulcer, and a 32-week-old diabetic ulcer. The subgroup of wounds having already existed for a minimum of 8 weeks showed a mean individual wound size reduction of 46%, illustrating wound healing progression even for chronic wounds.
Wound pain reduction
Wound pain is a challenging aspect for patients living with chronic wounds. At the end of this study, 23 patients (65.7%) reported less general wound pain compared to the first visit [Figure 5]. General wound pain reduced by 67%, from a mean of 2.69 to 0.88 (VAS scale, p<0.001). A total of five patients (14.3%) did not report any general wound pain during the study, which might be due to a sensitivity disorder, as four of these patients had diabetic ulcers (neuropathy is a common complication of diabetes mellitus; Sun et al, 2020). The fifth patient had a surgical wound.
During dressing removal, 87.0% of patients experienced no pain, 10.9% reported mild pain (1-2 on the VAS) and 2.2% reported a pain score >5 (VAS). The mean pain score during removal was 0.3 (VAS; the five patients without general wound pain were excluded from this calculation). Pain on removal was most pronounced in patients with leg ulcers, who also reported the highest baseline levels of general wound pain.
Application and removal characteristics
Clinicians rated the ease of dressing application highly in 100% of dressing changes and the ease of removal in 97.8%.
The dressing demonstrated good or very good conformability in 86.7% of applications. Adherence to the wound was reported as none in 55.8% of cases and little in 39.1%, with removal being atraumatic in 97.8% of instances. No bleeding occurred in 95.7% of removals; bleeding was classified as little in the remaining 4.3%. Wearing comfort was rated highly in 97.8% of cases.
Patient and clinician satisfaction
All patients and clinicians were either very satisfied (62% and 53%, respectively) or satisfied (38% and 47%) with the dressing. Treatment requirements were met in all cases.
Safety parameters
No device-related adverse events occurred, and no signs of infection were reported. All dressings could be removed in one piece. No device deficiencies were reported.
Discussion
Although wound exudate is a normal part of the healing process, excessive quantities or imbalances in its composition can lead to complications and delayed healing (WUWHS, 2019). Effective exudate management is therefore important to prevent negative outcomes and improve patients’ quality of life. Gelling fiber dressings absorb wound exudate, trap it within the matrix structure, and subsequently form a soft gel that maintains a moist environment conducive to healing. These dressings are widely used in wound care and have been extensively studied (Meaume et al, 2014; Chadwick and McCardle, 2016; Carrere et al, 2021; Joergensen et al, 2022; Fong et al, 2024; Klein et al, 2024).
This observational study demonstrated that Cutimed® Gelling Fiber effectively managed exudate in both acute and chronic wounds, leading to improved wound margin conditions. After the 4-week study period, wound size was significantly reduced, even in wounds that had persisted for several months. Additionally, patients benefited from reduced general wound pain and favourable application and removal characteristics (e.g. high wearing comfort and atraumatic, one-piece removal).
For efficient wound healing, it is also essential to identify and treat the underlying medical condition. For venous leg ulcers (VLUs), compression therapy is recommended as standard conservative therapy and is known to accelerate healing (Valesky et al, 2024). Therefore, it is crucial to select wound dressings that can effectively absorb and retain exudate while under compression. Both of these properties were demonstrated in laboratory testing for the study’s gelling fiber dressing (Heggemann et al, 2025), and further validated in this study. Exudate was successfully managed even when compression therapy was used.
Moreover, for treating VLUs, dressings that support wound cleansing or debridement are recommended (Valesky et al, 2024). Gelling fiber dressings are well-suited for this purpose as they possess autolytic debridement properties (Bishop, 2023), resulting in a reduction of sloughy tissue in the wound bed (Carrere et al, 2021; Klein et al, 2024).
If exudate is not managed adequately, prolonged exposure to moisture can cause maceration — a common complication, particularly in chronic wounds. Maceration can contribute to the enlargement of a wound area and increase the risk of infection, and has been shown to prolong healing time (Haryanto et al, 2017). While maceration warrants more focused research, adequate exudate management offers a way to prevent or reduce this complication (Whitehead et al, 2017).
Since gelling fiber dressings enable mainly vertical uptake of fluid (Richetta et al, 2011) and transfer exudate to a secondary dressing, they can be a valuable component in the prevention of maceration. In the present study, the percentage of wounds with macerated edges decreased, corroborating findings from previous clinical studies (Fong et al, 2024; Klein et al, 2024). Furthermore, gelling fiber dressings are conformable to the wound bed — a prerequisite for minimising dead space in the wound bed.
Complete wound closure has rarely been measured in gelling fiber studies, largely due to the limited duration for follow-up. However, the percentage reduction in wound area over a 4-week period has been reported as a reliable indicator of healing (Eriksson et al, 2022; Serena et al, 2024).
A chronic wound that demonstrates a 50% reduction in surface area within 4 weeks of standard care is likely to heal within 12 weeks under the same treatment (Eriksson et al, 2022). In the present study, the mean individual wound area reduction was 55%, with 55.9% of patients achieving at least a 50% reduction. Consistently, both exudate levels and the number of dressing changes decreased.
Similar gelling fiber dressings have shown positive outcomes in terms of wound size reduction in various wound aetiologies:
- 50% and 42% reduction within 6 weeks for exuding venous and mixed-aetiology leg ulcers, respectively (Joergensen et al, 2022)
- 35.4% reduction within 6 weeks for VLUs in a sloughy stage (Meaume et al, 2014)
- 18% reduction in length, 11% in width and 8% in depth within 4 weeks for hard-to-heal wounds (Fong et al, 2024)
- In diabetic foot ulcers, a correlation model identified a weekly reduction of 10% in area and 15% in volume (Chadwick and McCardle, 2016).
While partial wound closure does not automatically translate into direct benefits for the patient, patient-related factors such as quality of life and pain should be considered. Wound pain is one of the most cited concerns negatively affecting patients’ quality of life (Probst et al, 2023). In this study, a reduction of the mean VAS pain score by 67% demonstrated meaningful pain relief for the patients. Similar reductions in wound pain and improvements in health-related quality of life have been reported (Joergensen et al, 2022), while others observed only slight pain reduction (Fong et al, 2024).
As dressing changes are a frequent source of pain, the use of dressings that minimise trauma and pain are recommended (Woo et al, 2008). This study highlighted the favourable removal characteristics of Cutimed® Gelling Fiber, with atraumatic removal and no or low pain reported by nearly all patients. In contrast, studies on similar gelling fiber dressings have shown more varied outcomes, including a higher incidence of mild bleeding on dressing removal (Klein et al, 2024) or adverse events related to adherence to the wound bed (Fong et al, 2024). While the latter was associated with insufficient moisture in the wound bed, the gelling fiber dressing under evaluation may be used on dry wounds with appropriate precautions such as moistening the dressing and selecting a suitable secondary dressing to prevent desiccation, an approach that was validated in this study.
Limitations
Limitations of this study include its non-comparative design and small sample size. However, by applying broad inclusion criteria, a representative sample of wound care patients with a variety of different wound aetiologies and comorbidities were included, ensuring that the results reflect real-world data. At the same time, validity of subgroup analyses is limited by the small sample size. In addition, the possible effects of different secondary dressings were not investigated. Further controlled studies, including a larger sample size, may demonstrate further efficacy and cost-effectiveness of the dressing.
Conclusion
This study highlights the effectiveness and safety of a gelling fiber dressing when applied to low- and high-exuding wounds, both acute and chronic, in routine clinical practice. Key benefits observed included:
- Managing exudate for different wound types, even under compression, resulting in improved wound margins
- Enabling low-pain and atraumatic removal
- Reducing wound pain and supporting wound healing, independent of wound age or aetiology.
Ethics
This study was conducted in accordance with the ethical principles of the Declaration of Helsinki. Informed consent was obtained from all eligible participants after they were provided with an adequate amount of time to consider their study enrolment and before any study procedures were conducted.