Wounds have been referred to as the ‘Silent Epidemic’, with huge economic burdens on health budgets worldwide (Maheshwari, 2024). Around 15% of wounds remain unresolved even up to a year or more, resulting in a persistent burden to patients, their families and health systems (Lindholm and Searle, 2021). It is estimated that in a population of 1 million people, approximately 3,500 people will be living with a wound, with 525 of these living with a wound for over a year (Lindholm and Searle, 2021).
The negative effect of wounds on patients is widely documented, for example, the psychosocial effects of pressure ulcers, including odour, exudate and pain, can be severe and lead to various adverse outcomes, including embarrassment, chronic tiredness, self-imposed social isolation, depression and anxiety (Koumaki et al, 2023).
The presence of non-viable tissue in wounds, apart from being unpleasant and disturbing for the patient (Kalan et al, 2023), presents a barrier against effective wound healing, meaning that removal will facilitate healing (Percival and Suleman, 2015). Slough in the wound will prolong the inflammatory response, resulting in high levels of protease and pro-inflammatory cytokine production, act as a breeding ground for microorganisms and potentially biofilm formation, thus preventing the wound to progress towards healing by preventing the formation of granulation tissue, subsequent re-epithelialisation and interfere with wound contraction (Angel, 2019; Kalan et al 2023).
Moreover, matrix metalloproteinases (MMPs) play a vital role in the restoration of damaged skin (Kandhwalet al, 2022). However, excessive levels of MMPs have been associated with a significant delay in wound healing in chronic wounds of various aetiologies or even in stalled acute wounds (Lazaro et al, 2016).
In wound management, patient empowerment plays a role, especially considering the rising prevalence of wounds and limited resources (Moore, 2016). Patients should receive knowledge about their condition, and health and illness, resulting in patients having increased capacity to monitor and look after themselves (Moore, 2016). The importance of patient support was very evident during the Covid-19 pandemic due to closures of wound care clinics and outpatient centres (Cole, 2021). Supportive self-management, including patient education and wound management training, and skin management, can be adapted to promote safe patient self-care (Cole, 2021).
Callender et al (2021) discuss different methods of patient education and state that “patient-centred education for effective self-management is an essential component of the plan of care”. The authors suggest a framework to assist providers in implementing patient education by following the “5 As:”
- Ask patients about self-care
- Advise patients about the risks of nonadherence
- Assess patient readiness to follow recommendations
- Assist patients in creating goals and plans to implement recommendations
- Arrange for follow-up support (Kirst et al, 2017; Callender et al, 2021).
It is, however, important to evaluate and re-evaluate the methods of teaching and the patient’s demonstration of learning (Inott and Kennedy, 2011). One of the most widely used frameworks for evaluating learning outcomes is Kirkpatrick’s model, which consists of four levels: reaction — how the clients felt about the learning experience, learning — what they learned, behaviour — how they applied their learning and results — the outcomes of their learning (Steensma et al, 2010).
Polyabsorbent technology lipido-colloid fibre with silver dressing
The polyabsorbent fibres dressing (UrgoClean®, Laboratoires Urgo) absorbs exudate and traps sloughy residue (Meaume et al, 2012). The effective and rapid desloughing of the wound bed with these fibres was documented in a randomised controlled trial (Meaume et al, 2014) and proved to be superior to hydrofiber in its desloughing properties.
The addition of technology lipido colloid with silver (TLC-Ag) to the fibre dressing (UrgoClean Ag®, Laboratoires Urgo), provides a constant antimicrobial activity when in contact with the wound (Adolphus et al, 2015). Dalac et al (2016) conducted a prospective, multicentre, non-comparative clinical trial in patients with wounds at risk of infection, where, over a treatment period of four weeks of wounds mostly covered by sloughy tissue, the wound surface area was reduced by 32.5%, while 54.1% of wounds were debrided (defined by <30% of sloughy tissue covering the wound bed). Dissemond et al (2020) conducted a multicentre real-life, observation clinical study involving 2,270 patients with exuding wounds of different aetiologies at risk of infection or with clinical signs of local infection. An improvement in healing process was reported after a mean duration of treatment of 22 ± 13 days in 90.6% of cases, along with a reduction in all clinical signs of local infection, regardless of exudate level and proportion of sloughy tissues in the wound bed at baseline.
Technology-lipido colloid with nano-oligosaccharide factor treatment range.
The TLC-nano-oligosaccharide factor (TLC-NOSF) sucrose-octasulphate treatment range (UrgoStart Treatment Range, Laboratoires Urgo) has been shown to have MMP reduction properties, thus promoting faster healing rates (Münter et al, 2017; Meloni 2024). The treatment range has a wide range of evidence to support it, including results from two prospective multicentre clinical trials involving 88 patients with non-infected, moderately to strongly exuding wounds (Sigal et al, 2019). The use of TLC-NOSF with polyabsorbent fibres used in this clinical trial provided promising results regarding wound area reduction and wound healing rates, with the authors concluding that this novel dressing can provide clinicians with effective, safe, and simple solution for wounds at different stages of healing, until wound closure.
A systematic review conducted to identify the clinical evidence available on the TLC-NOSF treatment range, identified 21 clinical studies, varying from double-blind randomised control trials (Meaume et al, 2012; Edmonds et al, 2018) to real-life observational trials and case series (Dissemond et al, 2020; Munter et al, 2017), involving more than 12,000 patients. The authors concluded that TLC-NOSF treatment range provides an evidence-based solution for the management of wounds, enhancing wound healing, reducing healing times and increasing patients’ health-related quality of life, while being a cost-effective, and even cost-saving, treatment (Nair et al, 2021).
In a more recent systematic review (Meloni et al, 2024), it was shown that using TLC-NOSF treatment range as first-line treatment consistently resulted in significantly higher healing rates, shorter healing-times, and cost savings. TLC-NOSF also helped improve patients’ quality of life and is well tolerated and accepted.
Evaluation method
In the following cases, the patients’ wounds were initially managed with the polyabsorbent fibre dressings with TLC-Ag to reduce clinical signs and symptoms of local wound infection, and, thereafter, with the TLC-NOSF treatment range to promote healing. In the second case, due to restrictions of home visits during the Covid-19 pandemic, the patient was provided with education and training on changing the dressings himself. He was in contact with his general practitioner to provide information regarding progress and receive further instructions as needed.
Case 1
A 69-year-old male, bed and chair bound for the past 20 years due to a stroke, was referred to the wound practitioner for the management of two painful (visual analogue scale, Shafshak et al, 2021) and exuding Stage 3 pressure ulcers (NPIAP Staging; Rooney, 2021) on his buttocks [Figure 1a], resulting from extended periods in the supine position due to deterioration of his general condition caused by coronavirus disease. The wounds were previously managed with a silver wound spray.
Care of the wounds was provided at the patient’s home. The wounds were cleansed, and superficial debridement by curette was carried out. The polyabsorbent fibres with TLC-Ag dressing was applied to the larger wound to manage the higher risk of infection, while the polyabsorbent fibres with TLC-NOSF matrix dressing with polyabsorbent fibres was applied to the smaller wound to assist in keeping the wound clean and aiding faster healing. In both wounds, a TLC border dressing (a foam with silicone border) was applied as a secondary dressing.
Within 9 days, the larger wound was almost completely free of slough, and the smaller wound was showing substantial reduction in wound area [Figure 1b]. The same management was continued, and 2 weeks later, by 16/03/2022 [Figure 1c], both wounds showed further improvement with the larger wound showing healthy granulation tissue, and the smaller wound with further wound surface reduction. At this point, both wounds were treated with the polyabsorbent fibres with TLC-NOSF matrix.
By 19/05/2022 [Figure 1d], the smaller wound had completely healed, and the larger wound had a significant wound surface area reduction. Progression continued, as noted in 02/06/2022 [Figure 1e], and the second wound was completely healed by 28/06/2022 [Figure 1f].
Apart from the local wound management, position turning was advised and a hyper-oxygenated oil (Sanyrene, Laboratories Urgo) was applied to the intact skin to avoid further damage. Patient feedback confirmed Wound pain decrease throughout the treatment, with immediate reduction within the first 9 days.
In this case, the clinician opted for sequential management of the TLC-Ag and the TLC-NOSF matrix regimen to manage the risk of wound infection, prepare the wound bed and then accelerate granulation and epithelialisation. For the smaller wound, the TLC-NOSF matrix was applied as first line treatment to close the wound as fast as possible.
Case 2
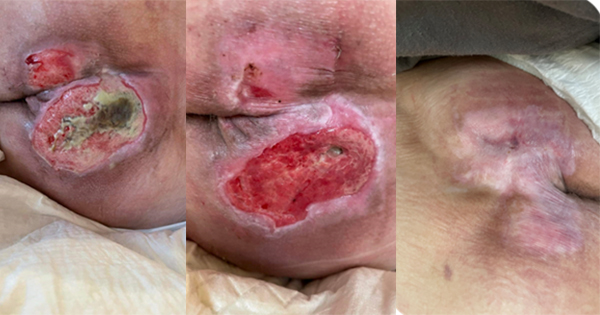
A 30-year-old paraplegic male was referred to the wound practitioner on 12/05/2020 for a non-healing, highly exuding Stage 4 pressure ulcer [Figure 2a]. The wound was previously managed with calcium alginate and silver hydrofibre dressings.
The wound cleansed with normal saline and then was packed with the polyabsorbent fibres TLC-Ag dressing that was fashioned in a rope, and a TLC absorb border dressing was applied as a secondary dressing, with dressing changes on alternate days.
As this case was during the Covid-19 pandemic, the wound care practitioner provided the patient with education on how to change the TLC-Ag dressing himself by means of using a mirror to see the wound. The patient was also in contact with his general practitioner throughout the treatment. This was necessary as there were strict restrictions for community nurses to visit patients and patient to visit ‘non-essential’ clinics.
By 12/06/2022 (4 weeks), the wound showed a healthier wound bed [Figure 2b], although still highly exuding. It was decided to apply a TLC-NOSF contact layer dressing as the primary layer to promote healing and the cavity was packed lightly with the polyabsorbent fibre TLC-Ag dressing to manage exudate and avoid local infection. The same TLC absorb border dressing was applied.
By 09/08/202, the wound size and exudate levels were reduced [Figure 2c]. At this point it was decided to pack the wound lightly with the TLC-NOSF contact layer dressing with the TLC absorb border dressing as the secondary layer. By 05/09/2020, the wound was completely healed.
A hyper-oxygenated oil (Sanyrene) and the TLC absorb border layer was then applied to protect the fragile skin to avoid recurrence.
For this case, the polyabsorbent TLC-Ag dressing, fashioned in a rope, was utilised to gently pack the wound and provide absorbency, but also to provide continuous cleaning and antimicrobial to overcome the signs and symptoms of local infection. Once resolved, the TLC-NOSF matrix provided the faster healing associated with this treatment.
As in the previous case, the patient was provided with support and education regarding prevention of further damage, such as pressure relief. The continuing management with the foam dressing and hyper-oxygenated oil prevented recurrence of the wound.
Case 3
A 69-year-old male was referred on 17/08/2020 with a painful, 7-day-old burn caused by a motorcycle exhaust. Up to that point, the wound was self-managed with a topical gel.
The wound was completely covered with devitalised tissue with periwound erythema [Figure 3a]. An ankle-brachial pressure index test was conducted to rule out lower-limb ischaemia (result = 0.9). Initially, the wound was cleansed, and sharp debridement performed. The polyabsorbent fibre dressing with TLC-Ag was applied to continuously clean the wound bed and provide an antimicrobial cover. The dressing was kept in situ by means of an elastic bandage from toe to knee joint.
The dressing was changed after 2 days (19/08/2020). Healthy granulation tissue was present and signs of inflammation in the periwound area were eliminated [Figure 3b]. At this point, polyabsorbent fibres and TLC-NOSF matrix border dressing was applied as the primary dressing. From here onwards, the patient was educated on changing the dressing himself every 3 to 4 days. It was opted to apply the TLC-NOSF matrix due to the risk of delayed healing (ABPI at cut off point of compromised circulation [ABPI of <0.9 is diagnostic of PAD (Wu et al, 2024]).
A follow-up visit was undertaken on 31/08/2020. The wound was almost completely epithelialised [Figure 3c]; a localised fibroma of approximately 1cm was cleaned with a curette. The same previous management was continued. The next follow-up was on 07/09/2020 where the wound was completely healed [Figure 3d].
With the application of the polyabsorbent fibre dressing with TLC-Ag, the wound was cleansed and local erythema resolved after only one dressing change. With the polyabsorbent fibres and TLC-NOSF matrix border dressing the wound was healed in a short period.
In this traumatic sloughy wound, with the sequential management of the TLC-Ag and TLC-NOSF, wound closure was achieved rapidly. The dressing was easy to apply, and the patient was empowered to manage the wound himself, with good outcomes.
In all the above cases, the clinicians were asked to evaluate the dressings for ease of application, ease of removal, non-adherence to wound, conformability, and acceptability. These were all rated 5 (with 0 being the worst and 5 being the most desirable). Acceptability, as rated by the patients were given the same score of 5. No adverse events were reported either by the clinicians or the patients.
Conclusion
The results of these initial cases supported the positive results that were obtained in large studies conducted using these dressings. These results were also consistent even when care was provided at the home of the patients, or even, if the patient is provided with education and instructions on how to self-manage his wound.
The positive results of the sequential use of these two dressings has also been recently published, providing even more evidence that using these technologies provides clinicians with effective and rapid results (Vaidya et al, 2024). The authors of this case series resonate the conclusion of Vaidya et al (2024) that the outcomes achieved in all cases were satisfactory, with a rapid reduction of clinical signs of infection, slough, exudate and pain, and a rapid wound closure, with no adverse events reported during the course of treatment.