“To err is human.” As Alexander Pope stated, humans make mistakes (Pope, 1711). In healthcare, mistakes can be as simple as a typo or as complicated as an incorrect diagnosis and treatment plan. Wound care is not exempt from errors, and errors can have a significant impact on patient progress and healing. Both authors serve as nursing experts in medical malpractice lawsuits in the United States. After numerous years of reviewing medical records, the authors have compiled a list of the ten most common and/or impactful errors in wound care, as well as remedies to correct and improve patient care and outcomes. We will progress from least impactful to most impactful.
1- Incorrect smelling spelling. Examples: “sloth in the wound bed”, “pus-sy drainage”.
Healthcare professionals can spend a significant portion of their lifetime training. According to the Cambridge Dictionary, ‘professional’ is defined as “a person who has the type of job that needs a high level of education and training” (Cambridge Dictionary, 2023). The spelling, pronunciation and medical records created by these professionals should reflect those years of training and use the correct terminology.
When assessing a wound, if the person assessing the wound sees yellow, brown, or grey inflammatory by-product in the wound bed, then it would be noted as “slough” (pronounced “sluff”, rhyming with “fluff”). If the person assessing found thick, yellow-white pus, describing the immune response of the neutrophil engulfing a microbe and being destroyed in the process (Dictionary.com, 2023), the person would correctly describe this presentation as “purulent drainage”. Purulent is the adjective of pus and is used to describe a wound containing pus.
Additionally, in the age of dictation and autocorrect, it is crucial to review your notes prior to entering to ensure words were not changed or modified. If using a drop-down menu, use the correct word or free text to ensure accuracy. It is not appropriate to choose the one that is the closest to what needs to be conveyed.
While this may seem to be an insignificant issue, as the reader would mentally correct the error, a jury does not. A jury sees the incorrect spelling and can easily question the education of the writer. Juries are not of your peers, and are not as likely to overlook a spelling error.
2- Measuring in food or coins. Examples: “pecan-sized wound”, “watermelon-sized bruise”, “nickel-thick collagenase”. (A nickel is an American 5-cent coin, approximately 2 mm thick.)
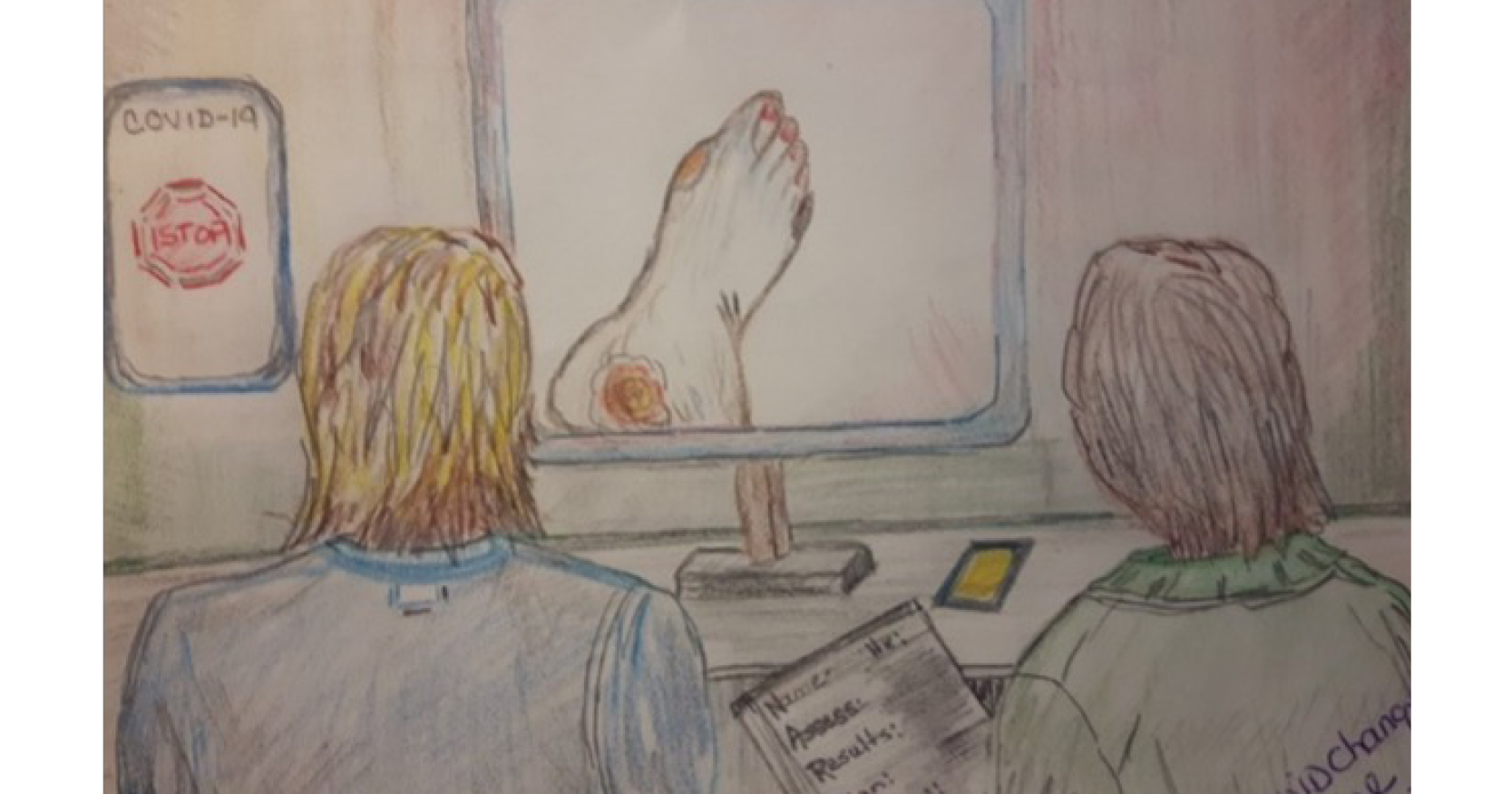
The only way medical measurement should occur is with metric measurements (centimetres, millimetres, millilitres, litres), to promote precision and consistency among medical professionals. The wound featured in Figure 1 was consistently described as a “small plantain”, despite clear differences in size and progress of the wound. There are several wound care organisations that explicitly state to measure wound dimensions in metric units.
To this end, metric measurement devices need to be readily available to any healthcare professional to facilitate accurate and thorough measurements.
Additionally, the wound is measured length by width by depth. Length is at the longest vertical length, width at the widest point, and depth at the deepest point. These measurements must all be consistently documented as length by width by depth.
3 – Using the pressure ulcer staging system to stage non-pressure ulcers. Examples: “unstageable venous ulcer”, “stage 2 skin tear”, “stage 4 diabetic foot ulcer”, “stage 6 surgical dehiscence with exposed hardware”
The National Pressure Injury Advisory Panel (NPIAP)/European Pressure Ulcer Advisory Panel (EPUAP) pressure ulcer staging system is to be used for pressure ulcers only. Diabetic foot ulcers have their own classification system, called the Wagner scale, while skin tears use the Skin Tear Classification System (STAR) classification and venous ulcers are classified using the basic CEAP system. Arterial ulcers and surgical site dehiscence must be assessed as intact, partial-thickness and full-thickness, as well as colours and erythema, presence of granulation tissue, slough or eschar, rather than the pressure ulcer staging system for depth and/or description.
When a wound that is not a pressure ulcer is staged with the pressure ulcer staging system, it can easily distort the true aetiology of the wound and misdiagnose the wound as a pressure ulcer. Furthermore, the treatment for pressure ulcers is not the same as other wounds, so there will be an apparent miscommunication in the plan of care, where a wound that is called a stage 4 pressure ulcer is being treated as a diabetic foot ulcer.
4 – No nutritional support. Example: stage 3 pressure ulcer that developed while the patient was on a 1,800 kcal diet. No new dietary orders, supplements or protein.
In our experience, malnutrition is a common cause of the failure of a wound to heal. Malnutrition can be easily addressed by asking for the dietician’s input and assistance in managing the patient’s nutritional status. Dieticians are experts in the field of nutrition and optimising nutrition. Therefore, it is in the patient’s best interest to consult with them when a new skin impairment arises, as they can identify protein needs, and other wound healing requirements. Whatever the patient was eating before will not be enough to repair the wound. Use registered dieticians to promote protein intake, as protein can be “hidden” in some drinks and ice creams.
5 – Not assessing weekly and use of “will continue to monitor”. Example: wound identified on June 1, first assessed on June 12, and assessed again on June 24. Nursing and wound care staff ending all notes with “will continue to monitor”.
The standard for wound care is a full assessment, measurements, drainage and progress upon identification and every 7 days thereafter, at a minimum. In a stable wound that is showing signs of healing, a formal assessment every 7 days is appropriate. However, a wound that is evolving or worsening, 7 days is too long and the patient can decompensate from the wound deterioration. Additionally, the formal assessment is used to identify any changes to the wound care treatment plan due to progress or deterioration. This formal assessment does not remove the responsibility during dressing changes to identify negative changes within the wound and update the plan of care at that time.
The use of “will continue to monitor” is often used to end narrative notes. It is unnecessary, as a significant amount of nursing care is monitoring for improvement, deterioration or development of a new condition. Therefore, “will continue to monitor” is essentially stating, “nursing staff will continue to do the bare minimum for the patient”. It is far more effective, and reflective of actual practice, to state, “will continue to assess”, as “assess” is an action verb, and “monitor” is a passive verb.
6 – Incorrect synopsis of wound and not changing orders to accommodate changing wound needs. Example: last week’s measurements: 5cm × 5cm × 0.2cm, 100% granulation. This week’s measurements: 7cm × 5.5cm × 0.4cm, 50% eschar, 50% granulation. Wound progress: healing. No new orders.
Based on the data provided, it is clear that this wound is not progressing toward healing, and in fact, is acutely worse. Accurate portrayal of the wound is crucial for the correct treatment of the wound, including advanced interventions, such as sharp debridement, and establishment of a positive trend in the healing process.
Additionally, the plan of care for the wound must be changed with acute deterioration, as the circumstance in which it developed will not be adequate for it to heal.
7 – Incorrect and inappropriate use of collagenase. Example: “collagenase until wound healed”; “apply collagenase to entire wound bed, both eschar and granulation tissue”; “collagenase to wound bed, top with mupirocin”
First, collagenase is an enzyme that breaks down human collagen. It was designed to be used to break down collagen in necrotic tissue and needs to be used for that circumstance. By its nature, the ointment will destroy nonviable tissue, and should be discontinued after granulation tissue is well established (Santyl Manufacturer’s Guide, 2023). Additionally, this ointment must be confined to the wound bed, as it will injure the collagen in the periwound skin. Collagenase is an enzymatic debriding agent and should not be used to close the wound.
If a wound has eschar or slough present, collagenase will take approximately 2 weeks to destroy that tissue, assuming it is applied correctly and consistently. Not all wounds with eschar and slough can afford to wait 2 weeks before correction. Wet and gas gangrene are not stable, and the person cannot tolerate waiting 2 weeks to treat these life-threatening infections.
In the third example, applying collagenase to the wound and then coating that with an antibiotic renders the antibiotic ineffective. The antibiotic cannot penetrate the collagenase, and therefore cannot reach the infection in the wound. It would be more effective to use sharp debridement to remove the infected necrotic tissue, and initiate either topical or systemic antibiotics after that, depending on the patient’s circumstance.
8 – Ignoring purulent malodorous drainage. Example: “wound now with odorous green-yellow drainage; will notify MD on rounds tomorrow.”
Purulent drainage is a sign of active infection. As stated previously, pus is created when neutrophils are destroyed after engulfing microbes. This infection can quickly spread to the bloodstream, leading to sepsis. Purulent drainage, especially abscesses, must be evacuated promptly to prevent the fluid collection from penetrating deeper into the patient’s soft tissues. Since the time of Hippocrates in ancient Greece, “pus under pressure”, or an abscess without a way to drain to the surface, must be opened by a physician and allowed to drain externally. Otherwise, the abscess will progress deep to the current location and create a worsening systemic response, up to and including septic shock.
Additionally, purulent drainage is not stable enough to wait for the 2-week delay for therapeutic use of collagenase. New onset purulent drainage requires an advanced provider to determine the next steps, including emergency department admission and/or hospital admission for emergent sharp debridement and possible systemic intravenous antibiotics.
9 – Waiting for the wound nurse. Example: wound is identified on Friday at 4pm, and Monday is a holiday with no wound care staff.
When a wound is first identified, the staff nurse who discovered the wound is responsible for measuring, assessing, attempting to classify, and developing a plan of care for interventions to treat the wound, (see tips 2 and 3). When a wound nurse is available, it is appropriate for a staff nurse to consult the wound nurse for assessment and development of a plan, so long as the wound nurse can assess the patient within a few hours.
Often, the wound nurse works approximately 40 hours, which leaves 128 hours without a wound nurse, per week. Therefore, staff must be trained and willing to begin the process of assessment, diagnosis, and interventions, without wound nurse input. To accomplish this, the staff nurses must have access to measuring devices, a dressing decision tree to guide appropriate topical treatment, and access to order upscaled mattresses, without waiting for the wound nurse to assess the patient.
There are many options to make this successful. One can be having multiple “skin champions” within the same area or unit to promote deeper understanding of wounds and increase the chances of one of them working during those other 128 hours. Alternatively, the facility can develop an algorithm to guide wound care decision-making after hours, so there is less delay between identification of the wound and initial treatment for the wound.
This is in addition to a wound nurse taking extended leave, absent leave, or prolonged absence for another reason. Staff nurses rarely need to identify an alternate care provider when on vacation or holiday, and this can be a novel idea for wound nurses, who do not have as many coworkers who can replace them for that time. This can feel like unfamiliar territory to a newly specialised nurse. Again, it is crucial for there to either be knowledge or a functional algorithm and instructions to ensure appropriate wound healing can occur when the wound nurse is not present.
Depending on the size of the facility, multiple wound nurses may be appropriate. If possible, it would be beneficial for the wound nurses to work varied hours throughout the day, to assist in providing more readily available wound expertise. For example, one can work from 6am until 2:30pm, and the other works from 9:30am to 6pm. This overlapping time allows for collaboration to occur while still providing increased access to experts.
10 – “Consult as needed” for an evolving deep tissue pressure injury. Example: A newly admitted patient with a suspected deep tissue pressure injury, with purple intact skin, is seen by the wound nurse. Upon assessment, the wound nurse writes the note stating “suspected deep tissue pressure injury, present on admission. Wound has not evolved currently. Will sign off. Reconsult as needed.”
In medicine, the consulting specialist signs off from the case when that medical speciality is no longer necessary, as the patient is stable and expected to improve without additional input from the specialist. Nurses are taught the “five rights of delegation”:
- right task
- right circumstance
- right person
- right direction and/or communication
- right supervision/evaluation.
Almost all deep tissue pressure injuries evolve into full-thickness, cavernous wounds within 7 days. During that time, the wound undergoes blistering, shearing, and full necrosis. The management of a new, evolving deep tissue pressure injury is not delegable to an inexperienced wound provider or staff nurse. Therefore, it is highly inappropriate for a certified wound expert to leave instructions to “reconsult if needed”.
Conclusion
While these ten top tips are not the only wound care errors the authors have seen, the frequency and severity of them are what brought them to make our top ten. Some can be easily fixed by verifying spelling, others require a significant change in clinical practice or a change in the facility itself.
These changes can be challenging and require buy-in from crucial stakeholders. However, both authors have repeatedly testified that a nurse’s number one priority is to advocate for the health and wellbeing of the patient.