1 – Prevention of contracture is key
Proper management of the acute burn limits the need for secondary contracture release. While not eliminating this need for eventual scar release, early excision and grafting has been shown to improve acute burn survival, outcomes, and need for revision (Mosier and Gibran, 2009). Supplemental therapies, such as physical therapy, early motion after initial grafting, silicone sheets and compressive garments, each play a critical role in minimising the need for symptomatic contracture development.
2 – The amount of “missing” skin is greater than what appears
A contracted scar the size of the patient’s palm often results in a wound three- to four-times that size once released surgically. Be ready with a proper donor site selection that is adequate in size. Always release the scar to determine the size of graft needed before harvesting the graft.
3 – The more tissue you can bring in the better the result
Full-thickness grafts often show a greater functional result than split-thickness grafts despite the greater difficulty in getting a “take” of a full thickness graft. Contractures relate to the amount of dermis that is missing and when you replace more dermis (as in full-thickness skin grafts) you mitigate the amount of contracture seen. Wound contracture seen after grafting full-thickness skin is less than split-thickness skin grafting in all types of wounds.
4 – Consider local flaps when possible, especially in well-defined scar bands
Scar contracture bands that are well defined cords of scar are often found when burns affect major joints, such as the axilla. If the skin adjacent to the burn is unburned and of high quality, consider designing Z-plasty flaps. This technique has greater success in permanently releasing the contracture for many reasons: thicker tissue is brought to the site, the flaps are vascularised and, thus, have greater survival, and Z-plasty flaps by design lengthen the site to which they are applied. A scar contracture band results from missing skin in a defined area and represents “too short” of an area of skin. Lengthening the band will result in greater mobility.
5 – Invite the occupational therapist to the operating room
The occupational therapist can gain a better sense of what you are trying to do as a surgeon by seeing what you do with the tissues first-hand. They can help you in the operating theatre by making a much better splint than you would likely make and begin the therapy relationship on day 0. Collaboration between the surgeon and the occupational therapist is key to identify range of movement (ROM) achieved intraoperatively and preferred positions for orthosis. Collaboration will result in both the surgeon and the occupational therapist having a better understanding of the other person’s goals and make each other’s results better.
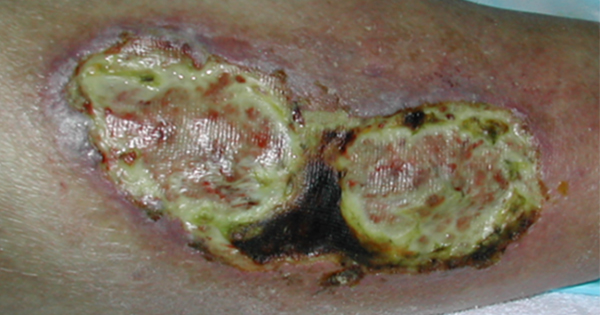
6 – Create a postoperative orthosis to properly position the patient during healing
Contractures are labelled opposite of the restricted motion. They identify the motion that the patient maintains. The patient shown in Figure 1 is unable to abduct his shoulder and is in an adducted position. This type of contracture is labelled a shoulder adduction contracture [Figure 2]. In clinical situations that allow for collaboration with a skilled occupational therapist or physiotherapist, custom orthosis fabrication is ideal to provide appropriate anticontracture positioning [Figure 3]. When custom orthosis fabrication is not available, over-the-counter options can also provide satisfactory positioning. Elbow extension orthosis or intrinsic plus position hand orthosis are widely available over the counter.
7 – Begin exercise early
In most cases, the patient is able to perform active ROM (AROM) exercises 5–7 days post operatively, if the incision is closed. In the early stages of tissue healing the goal of AROM is for muscle activation to reduce oedema and scar adhesions. As the incision heals increased ROM positions can be achieved. The patient should perform AROM often throughout the day (once an hour if possible) achieving the maximum ROM as tolerated by the scar and the patient’s pain. When the incision has healed well, passive ROM can be initiated. The patient’s joints should be stretched to the blanching point of the scar, indicating adequate tissue stretch for lengthening to occur. Stretching should avoid traumatic exacerbation of oedema.
8 – Educate the patient about anticontracture positioning vs positions of comfort
Scar tissue is biomechanically isotropic, which means it is organised with no specific orientation. Scar requires tensile forces to provide structural reorganising of the collagen fibres. After a burn or contracture release, patients often try to return to positions of comfort. These positions are detrimental because they do not put any resistive stretch on the newly forming scar tissue leading again to scar contractures. Custom orthosis fabrication and patient and family education about positioning is crucial to explain how proper positioning helps to introduce correct tensile forces to the scar as it forms and remodels. Anticontracture positioning uses orthoses, pillows and other informal positional aids, and AROM and passive ROM exercises to provide healing tissue with appropriate tensile forces to decrease risk of another contracture occurring. Common anticontracture positions can be referenced in Figure 4.
9 – Perform scar massage and scar care
Gentle scar massage can be initiated when the surgical incision is closed, approximately 3–5 days after sutures are removed. Scar massage helps to break up fibrous adhesions and maximise skin elasticity. Scars should be mobilised in each direction. Scar massage should be performed until scar has healed well and mobile. If the contralateral limb is unaffected it can be used as a comparison. Grafted and burned skin has limited ability to make its own natural oils requiring frequent application of lotions or oils as the scar matures and in the long term. It is also important to protect injured skin from sun exposure during the first year at least.
10 – Use the affected arm as much as possible for daily activities
This one is simple. Let daily life be therapeutic. Encouraging the patient to use their affected upper extremity during daily activities to maximise their functional ROM. Instead of avoiding activities that are difficult, thinking of those activities as therapy can help the patient to engage in increased repetitions of ROM. Participation is not only beneficial for functional ROM but also for patient self-esteem and independence. Patients can remove the orthosis to perform daily activities and return to wearing the orthosis at night and during inactive periods of their day.