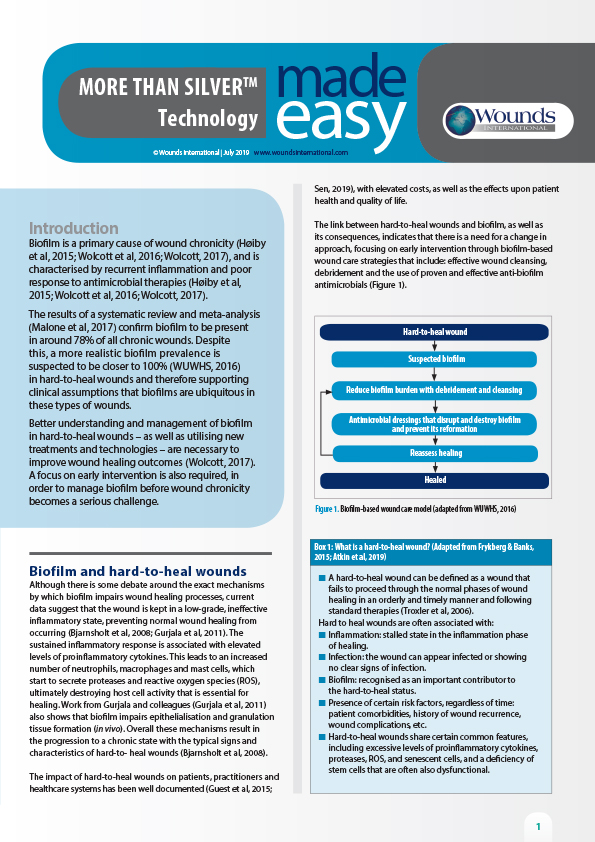
<p class="p1">Biofilm is present on the vast majority of chronic wounds and is suggested to be a key factor contributing to impaired healing. Biofilm provokes a heightened and prolonged inflammatory response with excessive proteolytic enzymes that degrade newly formed extracellular matrix and delay the healing process[2,3]. Biofilms are challenging to treat thanks to their innate survival techniques, which include antimicrobial tolerance. Physically removing biofilm from the wound surface through sharp debridement remains a cornerstone in successful wound management. However research has shown that no form of debridement or cleansing is likely to remove all of the biofilm and any remaining bacteria/biofilm has the potential to regrow, forming a mature biofilm in days. The strategy for treatment should therefore aim to prevent the reformation of biofilm following debridement while also managing the local wound environment to support healing. A novel technology is now available that combines the broad-spectrum, non-cytotoxic antimicrobial PHMB with a purified Type 1 native collagen matrix to manage bioburden and support healing across a wide variety of wound types. Data collected from the initial clinical utilisation of this technology highlights the clinical experience of managing challenging wounds of different aetiologies with this novel antimicrobial and purified collagen combination. </p>n<p> </p>