This study aimed to contribute to a growing body of literature focused on how the coronavirus pandemic in Canada was a shaping influence on the lives of respondents and the delivery of wound care services in the country over time.
Ethics and informed consent
The study adhered to ethics and consent protocols and was subject to review and approval by the Cape Breton University Research Ethics Board (Nova Scotia, Canada).
Methods
Frameworks and survey methodology
We utilised a qualitative descriptive survey methodology and follow-up interviews to collect perspectives of participants within various clinical contexts (Braun and Clarke, 2013; Salmons, 2015; Braun et al, 2020). We employed an online survey as the best fit for safe and timely data collection; see previous articles (Kuhnke et al, 2021a; 2022) for findings from datasets one and two.
Recruitment and participation rates
Following an identical process to datasets one and two, Wounds Canada emailed the survey to 12,204 potential participants. These are individuals who previously agreed to receive research invitations. The survey, instructions and informed consent were obtained. Open- and closed-ended questions were asked. Respondent numbers were survey 1 (n=245), 2 (n=67), and 3 (n=50). Participants were thanked for contributing.
Data analysis
Data were thematically analysed. We were mindful of recurring themes in each datasets and new data were compared, discussed and contrasted, and then analysed for similarities, differences and changes.
Findings
The following themes were identified:
- The most useful educational resources are those that are accessible in multiple formats and available synchronously and/or asynchronously
- Clear and detailed policies that provide a framework from which to assess, treat and manage skin and wound care are required
- Virtual technologies are increasingly embedded as part of the provision of care; however, problems and benefits were described
- Complex financial, personal and societal loads on individuals and systems are high and continue to result in losses.
Respondents want easy access to educational materials as part of their knowledge mobilisation of best practices
Throughout the pandemic, respondents routinely experienced barriers to the provision of wound care. As a result, many turned to educational resources as part of their efforts to find solutions. Respondents described the need for interprofessional collaborative (Canadian Nurses Association, 2022) education accessible to professionals providing skin and wound care. They shared the need for clinician, patient and specialist wound care education prior to the pandemic, and that the pandemic heightened the need for quality, accessible education. One clinician stated: “The education problem was always there, the pandemic just made it worse.”
Solutions identified by respondents to improve wound care education included: credible, accessible wound care practice videos; best practice guidelines; virtual courses for new staff; and support from health leaders. Respondents also described a need for time to complete comprehensive wound assessments and preventative skin health education. The following summarises what respondents described: “Physicians, nurses, specialists, and personal support workers require basic, consistent wound care education [that] must be offered regularly and individuals must be accountable for their ongoing wound care education competencies.”
Similarly, respondents identified the need for consistent, multi-modal, accessible patient/family education materials. They were asked to describe their use of the recently developed Wounds Canada — Care at Home Series (Wounds Canada, 2020). In hospital settings, respondents reported the following: “We linked the series to the library home page for staff use. We used the surgical wound, swollen legs, venous and diabetic foot handouts [and] we used them with clients when relevant.” In the community setting, one respondent commented: “The tools were helpful with education. I used them for patients being discharged home with no home care support”.
Respondents identified the need to develop patient-centred (Registered Nurses’ Association of Ontario, 2015) educational materials for all care settings. Specifically, they requested the following topics be developed: continence care, use of briefs, skin tears, pressure injury prevention, assessment and management, lymphoedema, ostomy care, burn wounds, surgical drain care and skin care for persons using drugs. In addition, they identified the need for patients and families to be educated using patient-centred versions of pressure injury and diabetic foot risk screening tools. Furthermore, they identified some patients and families as knowledgeable and capable of screening for risk of skin changes between the wound care clinician visits. Respondents also stated that families and clients are sometimes reluctant to provide self-care, yet they perceived them as capable of being more independent.
Respondents are clear in their understanding of its importance in the prevention of wounds, assessment, treatment and management of skin, and wound care issues.
Clear and detailed policies
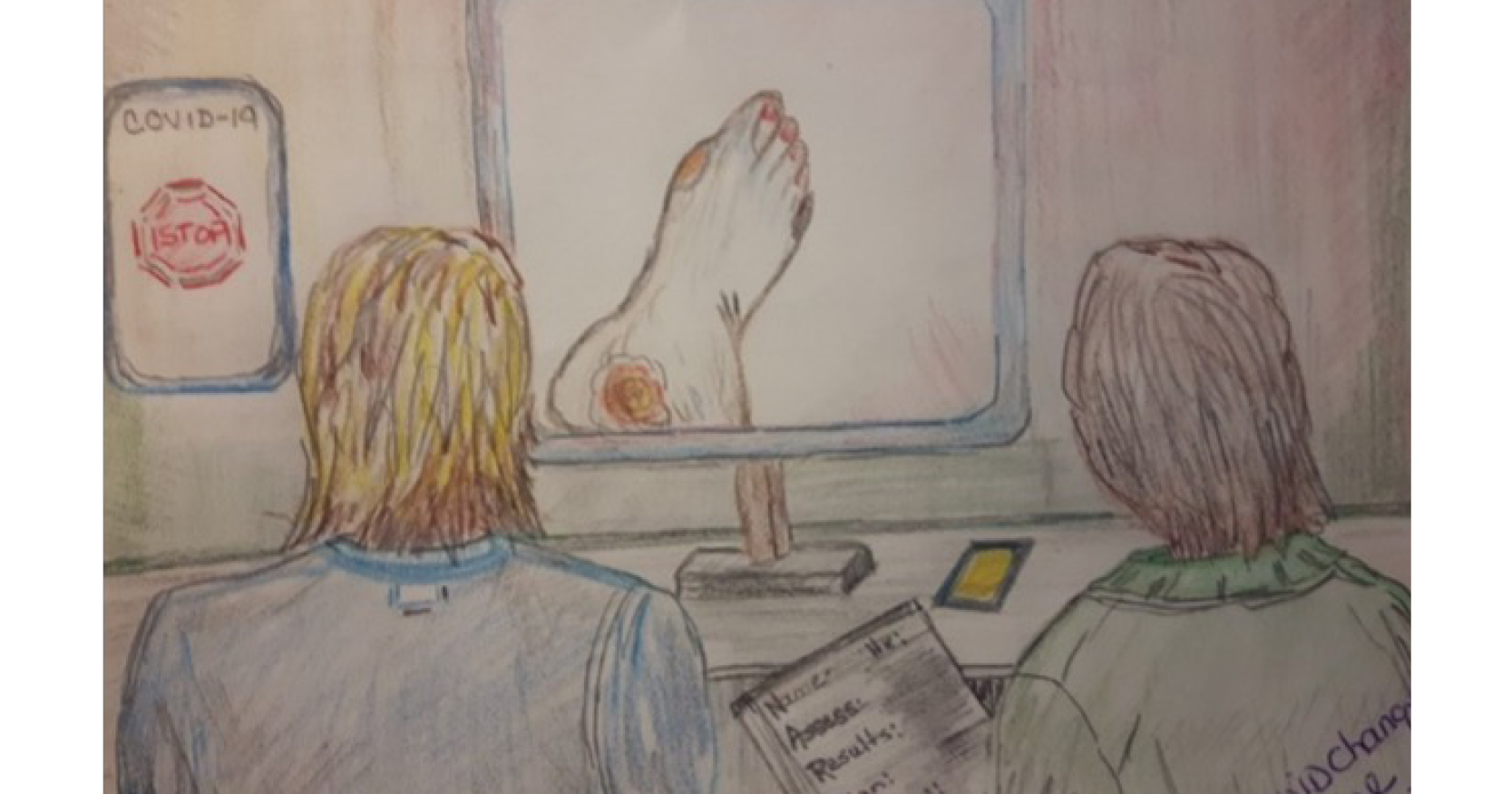
Respondents described varied polices guiding access to skin and wound care across health regions and reported tensions and frustrations with reduced wound care services. They also described how some wound care clinics had polices in place, or developed them, which allowed teams to continue to offer care, and others moved wound assessments to virtual e-platforms without delay [Figure 1]. One clinician stated: “We triaged the patient by phone and obtained a detailed health history. We completed the second and subsequent visits via an e-platform; though not ideal, we kept the wound care service going.”
When clear policies were not in place, tensions mounted. For example, some clinics operated “less often, some were closed due to staff shortages, and others lacked skilled wound care clinicians to manage the clinics”. When clear policies did not exist or were in flux, respondents thoughtfully attempted to influence policy as part of their efforts to provide patient-centred care. For example, to maximise limited clinic time, respondents encouraged physicians to “learn to triage and assess basic wounds before sending patients to the wound clinic service as some referrals were unnecessary, or the patient/family could have managed the care”. Another respondent also described community clinics as “experiencing an increase in referrals, yet managers, did not increase staffing ratios or provide supportive wound education because policies did not exist to guide them, or they lacked access to available staff”.
In addition, respondents identified gaps in wound care service delivery, particularly in relation to policies that deemed wound care clinics non-essential. One clinician remarked: “Wounds did not go away because of the pandemic; risks of peripheral artery disease and diabetes did not go away, wounds got worse because clinic closures interrupted the provision of care! Why were policies put in place that identified clinics as non-essential?” Another stated: “I have a client with diabetes, the person ended up waiting for an assessment for 6 or more weeks, resulting in an amputation prior to having any home care services; how does this happen?” [Figure 2].
Respondents identified individuals needing specialised diabetic foot care who experienced difficulties when attempting to access care in a timely manner. One stated: “We have no access to chiropodists for patients with diabetes or nurses specialised in wound, ostomy and continence care; we have less resources than before the pandemic.” Another said: “We are stretched so thin, there are not enough of us … we are lacking qualified staff resources to operate our clinics; therefore, the clinics close or have limited hours.”
Virtual technologies are increasingly embedded as part of the provision of care
Barriers and benefits to the incorporation of technology were described. Respondents stated there were interruptions in care, however, technology provided alternatives. Some respondents described their use of and access to technology (e.g., telehealth, photography) as established before the pandemic. Others described an immediate need to implement the use of technology because face-to-face visits were prohibited. Those who had no or limited previous experience with the use of technology described how effectiveness improved over time as safeguards to protect the data were put in place, education was made available (providers, clients) and technology infrastructure was implemented.
Some respondents in rural settings described no support for use of photographs and associated communication tools to use with physicians or specialised wound teams. Others indicated that the technology allowed consistent and timely access to specialists and physicians. There was another who stated: “Everything remained the same during COVID in terms of wound care. Not much changed except for leaders’ and managers’ greater understanding that early recognition of wounds is key to avoiding local and systemic infections.”
Community-based home care
Respondents commented on the benefits of technology, with one stating: “It brought specialised care into individuals’ homes.” Another noted: “A year into the pandemic and we don’t use or have technology to record or pass along wound care pictures or monitor changes.” Another explained: “The utility of virtual wound care is limited. You can’t debride a wound over the phone.” Meanwhile, two NSWOCs noted: “We do not have trained nursing staff, other than part-time NSWOCs. Mostly they perform conservative sharp wound debridement, lower-leg assessments including ankle-brachial pressure index measurements, and total contact casting … our virtual practice as an NSWOC was almost impossible to do as we were the only ones trained in these specialities, so we did home visits as able.”
Months into the pandemic, respondents noted virtual wound visits continued to be challenging. Respondents described “upper management as slow to adopt available wound technologies, while others adopted without team input”. Nurses, pressured to quickly learn technologies without proper education, did not all adapt well. Community respondents described pressures when conducting mandatory home visit times. One stated: “Visit times were often imposed; we had to be present at specific times and days in order to facilitate a physician or NSWOC consultation. Our impression was that many of these consults were not up to par with face-to-face visits. We were often frustrated by stagnant or worsening wounds that would have benefitted from debriding, offloading or vascular care that community nurses cannot provide. The client did not need a virtual visit, the client needed advanced wound treatment and management.”
Complex financial, personal and societal loads on individuals and systems are high and continue to result in losses
Efforts to establish and maintain work-life balance continued to be a complex issue. Respondents stated that prior to the pandemic they worked to create some semblance of work-life balance. Throughout the pandemic, precarious efforts to positively impact work-life were negatively impacted and stress continued and increased. For example, some providers described continued distress related to access to and use of personal protective equipment. Others described stress related to whether patients were vaccinated. They also mentioned stress associated with the constant need to stay abreast and implement constantly changing pandemic communiques. They described mandates over time, lack of qualified wound care respondents, inability to recruit and fill staff vacancies and reductions in wound clinician staffing ratios.
With respect to balance at home, respondents recounted increased tensions with partners, children, family members and friends, while some experienced the end of long-term relationships. Others reported anxiety and sleep interruptions with multiple changes in practice settings and unpredictable changes to clinical responsibilities. “I am too exhausted both physically and mentally when I arrive home to deal with chores related to my family after cleaning (COVID-19 protocols) clients’ homes, touch points and my car,” one said. Participants also described how the shift to working from home impacted their efforts to create work-life balance: “Weblinks and internet access eroded my home and family time”.
“I worry that a client’s wound will deteriorate. I know how quickly the need for an amputation can ensue,” said another. I had a scenario where I was unable to visit due to COVID. My client needed urgent care for a new wound that had developed on the top of the foot and at the base of her toes. As the only wound care nurse, I could not send someone in my place and could not visit for 5 days. I saw this client before and knew an immediate response was needed. It was so stressful to me, the clinic, the client and my family.”
Another clinician stated: “I am finding practice more challenging. In the early stages of the pandemic, I lost my childcare and had to work from home while caring for a 2-year old”. A manager who also practised clinically said: “I have been working a lot more at home to catch up on administrative duties and chart; we were forced to stay open longer, we were short-staffed, and we had an increase in volume of complicated wounds”.
Adapting and self-care
Respondents described some of the self-care strategies they attempted to implement in efforts to deal with the complex and often-mounting stressors. One said: “I am more aware of caring for myself. I am enjoying my family more as we work and consult from home … I do not look at my work phone on my days off.”
The key message revolved around care for self, especially mental and physical health. Several respondents mentioned closely monitoring and then limiting the number of hours they used their phones or laptops, including “leaving non-urgent paperwork to the weekend instead of trying to complete everything on weekdays and working 12-plus hours.” One clinician stated: “I just had to leave work at work. I don’t look at emails over supper or before bed; if I do, I don’t sleep.” Others described the importance of insisting on days off. Some were unable to maintain balance and as a result left their jobs: “I could not keep working on the floor as a wound care nurse; I’m burnt out.”
Discussion
These data from the final survey of a serial, qualitative pan-Canadian study highlight the perspectives of wound care respondents a year into the global pandemic. The study was conducted at a time when respondents’ ability to visit, assess and provide treatment face-to-face was sometimes prohibited and, most often, complicated and deemed non-essential (Public Saefty Canada, 2021). The closure of outpatient wound clinics and wound- and foot-care services interrupted the provision of care.
Issues related to the availability of appropriate levels of trained staff and those trained in wound care were consistently reported. A lack of trained and available staff often resulted in increased levels of stress for respondents. Respondents continued to relate that trained wound care staff were lacking and time was limited to properly deliver skin care related prevention strategies and wound care.
Respondents were concerned about client’s overall health, especially those with complex wounds underpinned with multiple comorbidities — diabetes (infection, amputation), peripheral arterial disease, mental health issues, renal disease — and this concern was heightened with the pandemic (Oropallo, 2021; Lu et al, 2022). Armstrong (2021) states the delay of chronic wound care during the pandemic has created increased hospitalisations, delay in treating infections, and increased amputations. As many wound care services in Canada were closed or offered limited services when deemed non-essential, respondents sought to advocate for clients and tried to adopt new virtual ways of practising.
Broadly, there were two responses to what was regularly described as constant changes and stressors. The first is best described as creative adaptation. The second response can be broadly described as acceptance. After multiple efforts to provide care and maintain some level of work-life balance, some respondents changed jobs, took leaves, or left.
Committed professionals and educational programmes
Similar to the literature, respondents described the need for ongoing, accessible skin and wound care education for healthcare providers. They also noted that such education was limited even prior to the global pandemic. The pandemic and the subsequent and ongoing changes to the provision of care heightened inequities in wound education (Britton et al, 2020). Though wound care education was moved to online formats, it did not necessarily mean respondents had time to participate due to caseloads, staff turnover, and redeployment. Respondents detailed the growing need for advanced wound care webinars, skills and knowledge videos, and education focused on proper use of wound care products. They also stated that managers and leaders need to support their ongoing education and competencies development.
Survey respondents also commented on education for patients and caregivers. Specifically, they noted a need for patients and caregivers to take a more active role in skin assessment and wound care as they viewed patients and caregivers as reluctant, yet capable. They deemed the Care at Home Series (Wounds Canada, 2020) effective; however, they requested and identified additional topics for development.
Technologies and the provision of wound care services
The use of technology, including benefits and challenges, was consistently described across the studies. It is interesting to note that prior to the pandemic, some professional organisations such as the Canadian Medical Association (CMA, 2021), the College of Occupational Therapists of Ontario (College of Occupational Therapists of Ontario 2017) and the Registered Nurses’ Association of Ontario (RNAO, 2017) had or were in the process of establishing virtual care practice recommendations. To support patients and families, the CMA established a handbook (CMA, 2020) with strategies to support successful patient-centred virtual visits. The RNAO and Associated Medical Services also published a report (RNAO and Associated Medical Services, 2020) focused on the role of compassionate client care. The recommendations within the report were not referred to by any of the study participants over any of the three surveys. This led us to wonder if there had been any uptake of the recommendations prior to or during the pandemic.
In relation to technology, internet access, familiarity, privacy, access to hardware and software, and education were some of the concerns raised by respondents for themselves, their clients, and families. The data support the notion that for respondents practising in urban settings, the use of technology did improve the care provision in terms of being able to assess a client using devices. Though technology was part of their practice, they consistently identified the quality of photographs as being poor, therefore making the technology less effective. Similar to the research, for some respondents familiar with wound technologies prior to the pandemic, they continued to embed technologies in their care plans (Wentink et al, 2018; Leonardsen et al, 2020).
Respondents practising in rural and remote communities who live with minimum service levels and lack infrastructure and or access to devices (purchase costs — phone, tablet, computer, internet service fees) did not report similar uptake of technologies. Though the government states there is a mandate to have Canada connected through technologies, participants spoke of the barriers (Statistics Canada, 2021a; Government of Canada, 2022). As well, persons who live in vulnerable situations (those living with wounds and with multiple comorbidities; frail, older adults; persons using drugs and those with mental health disease and/or with no advocate (list not inclusive) often were outliers in terms of accessing and benefiting from the common technologies used in the provision of healthcare services. More research is needed to understand these barriers and solutions.
Work-life balance was a constant struggle
Similar to Adams and Wall (2020) respondents described their efforts and challenges when attempting to maintain work-life balance. They described the importance of engaging in self-care and wellness practices (Knighton, 2011; Kuhnke et al, 2021b). They also identified compassion fatigue (Upton, 2020) when caring for patients with complex wound issues. Findings from our study were similar to current literature exploring healthcare workers’ wellness during the COVID-19 pandemic. LoGiudice and Bartos (2021) studied nurses’ experiences during the first wave of COVID-19; nurses were highly stressed and resilience was low when they practised with limited time to prepare for patient caseloads. During the pandemic, Statistics Canada (2021b) studied healthcare workers reporting:
one-third reported poor to fair mental health
those working with COVID-19 patients reported worsening mental health
consistent access to PPE [personal protective equipment] improved workers’ mental health and lowered stressors.
In Ontario, the COVID-19 Science Advisory Table and its Working Group on Mental Health reported increasing burnout related to “workplace factors, such as workload, interpersonal conflict, moral distress, administrative burdens and documentation, and provider factors: such as low self-efficacy, emotional exhaustion, reduced sense of personal accomplishment” (Wounds Canada, 2020). Data from this study support all the findings noted above. From this, we understand there is an acute need to provide complex support as identified by respondents if they are to work effectively throughout a pandemic.
Conclusion
This paper reports on the final survey results of a study designed to learn from the experiences of wound care respondents working to meet the needs of patients during the pandemic. Respondents’ ability to deliver skin and wound care services was never stable or consistent. Multiple policy changes, technology benefits and limitations, availability of PPE and ongoing education, stress levels and efforts to provide self-care shaped how wound care was provided. Survey respondents not only described their own experiences, but also became a voice for vulnerable populations and their families who needed access to skin and wound care.
Respondents expressed concerns and a lack of understanding as to why skin and wound care services were deemed non-essential. This will be an important question to answer as we learn from past experiences and prepare for future regionalised, national and/or international outbreaks that impact the provision of wound care services. Moreover, if we are to support, rebuild and grow our wound care teams, we must attend to workplace stress, work-life balance and education. We would suggest if these issues are not deeply understood and addressed using new, supportive policies, then we risk losing more respondents, resulting in a decline in the provision of care.