The skin is the largest sensory organ in the body and is critical for survival due to its role in protecting the individual from the external environment and keeps harmful influences at bay. When the skin is destroyed, damaged, or broken, a regulated sequence of biochemical activities begins to repair the damage through wound healing (Nguyen et al, 2009), a normal physiologic process accomplished through four precise and highly programmed phases of hemostasis, inflammation, proliferation and remodelling. The physiological regulation of skin wound healing is a complex process involving many cell types and mediators interacting in a highly complex sequence.
Thus, for a wound to heal successfully, all four phases must occur in the correct sequence and time frame. As a fragile process, several factors such as age, nutrition, infection and the presence of comorbidities can all interfere with one or more phases of this process, resulting in the formation of chronic or non-healing wounds. Frykberg and Banks (2015) defined chronic wounds as wounds that fail to progress through the normal phases of wound healing in an orderly and timely manner. Though there are different definitions of chronic wounds based on time, several scholars agree that any wound that does not achieve re-epithelialisation between 6 and 8 weeks is a chronic wound (Singh et al, 2004; Leaper and Durani, 2008; Han and Ceilley, 2017; Institute for Quality and Efficiency in Healthcare, 2018).
More often than not, chronic wounds frequently stall in the inflammatory phase and despite differences in aetiology, most chronic wounds share certain common features at the molecular level, including excessive levels of proinflammatory cytokines, proteases, reactive oxygen species and senescent cells, as well as the existence of persistent infection and a deficiency of stem cells that are also frequently dysfunctional. Chronic wounds are becoming a public health concern as their prevalence rises and treatment becomes more difficult. As such, they impose a significant economic burden on the healthcare system in general and patients in particular (Rice et al, 2014), with serious implications for the quality of life of those affected. These wounds, if left untreated, result in a vicious cycle of systemic dysfunction.
Therefore, expediting healing becomes paramount and wound care becomes imperative, in order to speed up the healing process by maintaining asepsis and preventing from re-injury. To that end, chronic wound care has evolved into its own specialty, with providers now employing advanced wound management therapies.
These treatment options have been used as stand-alone or combination therapies, but current regimens are insufficient, necessitating the use of adjunctive therapies in the treatment of chronic non-healing wounds. This includes, but is not limited to, the use of electrical energy as a medical treatment (IEEE, 1997).
Electrotherapy and other biophysical modalities have been used as adjuncts to conventional wound care by physiotherapists and other clinicians worldwide for over 5 decades. Sadly, despite extensive literature supporting the use of electrotherapy and physical agents in managing chronic wounds, physiotherapist rarely get involved in management of patients with chronic wounds in Nigeria. This unwelcome situation is thought to be caused in part by a lack of adequate wound care knowledge and/or poor interprofessional synergy within the Nigerian healthcare system. This has the potential to have a negative impact on outcomes in patients with chronic ulcers because physiotherapists who are not involved in wound care are a significant untapped resource with great potential for promoting wound healing (McCulloch, 1998).
As a result, it is critical to determine physiotherapists’ knowledge and use of electrotherapy in the management of chronic wounds. This is the concern that this study aims to address.
Methods
This is a cross-sectional study in which a self-administered questionnaire was distributed to 76 physiotherapists (38 males and 38 females) from the three tertiary institutions within the Enugu Metropolis. The questionnaire was a structured closed-end type that assessed respondents’ social demographics, knowledge of electrotherapy in wound management, involvement in wound care and barriers to participation in wound care. Return of the completed questionnaire was interpreted as consent. Ethical approval was not obtained as this was not required. Convenience sampling was used to select an equal number of male and female physiotherapists in clinical practice. The study excluded non-practicing and academic physiotherapists.
Statistical analysis
SPSS version 21 (SPSS Inc, Chicago, Illinois) was used to analyse the data, which included descriptive statistics and pearson chi-square at the 0.05 level of significance.
Results
The general characteristics of the study participants are shown in Table 1, with equal participation of male and female physiotherapists. The majority of respondents (40.8%) were between the ages of 31 and 40, had a Bachelor’s degree as their highest educational qualification (69.7%), and were senior physiotherapists (31.6%) with more than 5 but less than 10 years of practice experience (40.8%). The majority of respondents (56.6%) worked at federal university teaching hospitals and specialised in musculoskeletal physiotherapy (40.8%).
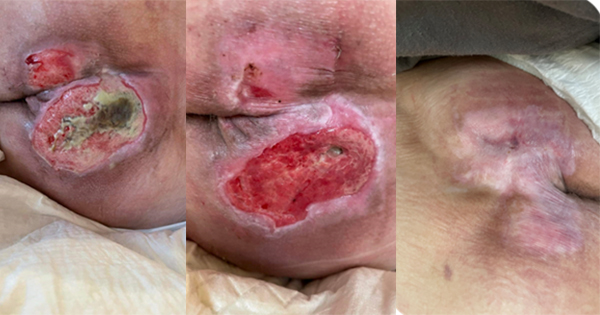
Nearly all (98.7%) respondents had a good understanding of the role of electrotherapy in the management of chronic wounds, with school being the most common source of information (42.1%) and ultraviolet radiation therapy (UVR) being the most commonly used modality (42.64%). There was generally good knowledge (75%) of the types of wounds that respond to electrotherapy, a fair knowledge of contraindications (55.2%; Table 2), but a lack of understanding of complications, precautions (46.3%), wound assessment tools (7.9%) and wound dressing techniques and options (18.4%) [Figures 1–3]. Table 3 shows that 27.6% of the subjects had been involved in wound care and had used electrotherapy at least once, with only 11.8% currently actively involved in wound care. 61.9% of respondents currently invovled in wound care have completed bridge or transitional degree programmes.
A chi-square analysis of relationships reveals no statistically significant (P<0.05) associations between respondents’ knowledge and job rank (P=0.27), number of years of practise (P=0.07), educational level (P=0.45), or job rank, use of electrotherapy (P=0.19) or active participation in wound management (P=0.63) [Table 4].
Discussion
The purpose of this study was to determine physiotherapists’ knowledge, use of and barriers to electrotherapy in the management of chronic wounds, as well as to establish associations or not between physiotherapists’ knowledge of electrotherapy and their use in wound care. Research findings suggest that a large proportion of respondents have a good knowledge of the role of electrotherapy in the management of chronic wounds, with formal education being the most common source of information. Furthermore, this study found that participants had a good understanding of the types of wounds that respond to physical therapy and a fair understanding of contraindications. This finding is not surprising given that previous research has shown that physiotherapists have a generally good knowledge of wounds and role of electrotherapy as an adjunct to standard wound care. Recognising the important role of physiotherapists in promoting chronic wound healing, the American Physical Therapy Association and the Commission for Accreditation of Physical Therapy Education have made this a key requirement for graduation into the physical therapy profession. Other scholarly works, such as those of McCulloch (1998) and Clarkson et al (2019), demonstrated that physiotherapists were well-versed in electrotherapy and its application in wound care.
Feily et al (2006) reported that physiotherapists have many interventions at their disposal to improve wound healing outcomes in chronic and complex acute wounds. This report demonstrates that physiotherapists are well-versed in electrotherapy in wound care; otherwise, these interventions would have been difficult or non-existent.
Despite having a good understanding of electrotherapy, wound types, and contraindications, the study found that most respondents had a poor understanding of precautions and possible complications, wound assessment tools, dressing selection and techniques. This study contradicts existing literature that portrays the physiotherapist as a key player with the necessary knowledge and skills in wound care. This issue is demonstrated by the existence of several wound clinics owned or run by physiotherapists all over the world (O’Sullivan-Drombolis and Orr, 2011; Cordrey, 2014), as well as the existence of clinical practise guidelines for the role of physiotherapy in wound management (VCH, 2010; APTA, 2020).
These contradictory findings may be the result of academic and training curriculum deficiencies, clinical experience, or both. It is expected that if this were not the case, Nigerian physiotherapists’ knowledge of their roles in wound management would go beyond a general understanding to include more specific information about various other aspects of wound care that can be translated into clinical practise to improve patient outcomes.
The scarcity of scientific articles or data from Nigeria supporting the use of electrotherapy in wound care reflects this lack of knowledge about contraindications, precautions, and complications. It is also possible that these findings are the result of a lack of necessary equipment, which prevents physiotherapists from practicing.
Another objective of this study was to determine the use of electrotherapy modalities in wound care as well as physiotherapist involvement in wound management. The findings revealed that a small percentage of respondents (27.6%) had been involved in wound management at least once, with only a few (11.8%) currently actively involved in wound care. Despite widespread recognition of physiotherapists’ role in promoting chronic wound healing, this finding was not unexpected, as it corroborated previous studies that found underutilisation of physiotherapy and biophysical agents in wound healing. O’Sullivan-Drombolis and Orr (2011) reported that the role of physiotherapy in wound care in Canada is much less developed, when compared to the United States and other countries, and as a result, physiotherapists’ involvement in direct wound care is significantly reduced.
Poor administrative support, ineffective education and a lack of cooperation from physicians are cited as some of the barriers preventing the translation of knowledge into practice. If this is the case with some of the world’s leading healthcare systems, it stands to reason that a developing country like Nigeria will be less likely to be at the forefront of implementing these guidelines. As with previous research, the reduced involvement of Nigerian physiotherapists in wound management observed in this study may be attributed to insufficient knowledge, reduced interest or interprofessional conflicts. The findings of this study, however, contradict those of Kloth (2009), who observed that clinical wound management has evolved into a practice speciality for practitioners from a variety of healthcare professions over the last four decades.
Since the early 1980s, physiotherapists have been major players in wound care teams in the United States, and their involvement is growing in countries such as Canada, Poland, Singapore and Thailand. Similar to findings from this study, Kloth (2009) also observed that in many other developing countries, few physiotherapist’s are involved in direct wound care. Increasing knowledge base, developing clinical guidelines, and promoting interprofessional synergy may thus help to improve physiotherapist involvement in wound management, thereby improving patient outcomes
Finally, this study went ahead to explore the associations between respondents’ knowledge and rank, number of years in practice and use of electrotherapy in wound management. The findings revealed no significant relationships between the variables under investigation [Table 4]. This finding differs from previous research, which found significant positive associations between knowledge and practise (use). Yahya et al (2012) discovered a significant relationship between cardiovascular disease knowledge and preventive practises. Similarly, Dowell (2015) discovered statistically significant correlations between knowledge and health practises.
According to this, it is expected that a high level of knowledge of physiotherapists’ roles in wound care will result in significant positive correlations with practice. However, this was not the case. This failure to observe significant relationships between knowledge and rank, practice, and experience may be the direct or indirect result of previously identified barriers to practice [Table 3], including but not limited to scope of practice, lack of interest, poor interprofessional relationships and paucity of human and material resources.
This stands to reason given that the majority (61.9%) of those actively involved in wound care are professionals who have either completed bridge and transitional programmes or other continuing education programmes. As a result, because policymakers play a significant role in curriculum development and licensure requirements, improving existing curriculum will significantly increase physiotherapist involvement in wound management.
Conclusion
Finally, as a member of the multidisciplinary wound team, the physiotherapist must make an effort to acquire the necessary knowledge and skills while fostering positive interprofessional relationships in order to improve outcomes for patients with chronic wounds. Since respondents identified improving training curriculum (43%), improving knowledge through continuing development programmes (35.5%), transitional or bridge programmes (48%), and improving interdisciplinary partnerships (20%) as major areas for improvement, it is recommended that these areas receive priority consideration in developing guidelines and policies that will result in better practise.