The healing of acute wounds usually follows a fixed structured physiological pattern. This pattern consists of four different phases (haemostasis, inflammation, proliferation and remodelling). If this pattern is disturbed, the healing process is delayed and the wound may become chronic, which may result in ‘hard-to-heal’ or complex wounds (Sorg et al, 2017). Causes of delayed wound healing include: prolonged inflammatory stage, failure of normal growth factor synthesis, overexpression of protease activity and/or increased disintegration of growth factors due to lack of normal anti-protease inhibitor mechanisms (Barbul et al, 2015; Calis et al, 2020).
Introduction
Wound dressings play an important role in local wound care and contribute to achieving an antimicrobial environment where necessary, a balanced moist wound bed and protection of the periwound skin (Winter, 1962; Butcher, 2000; Cutting and White, 2002; Sharman, 2003; Burton, 2004; Cameron, 2004; Guo and DiPietro, 2010). It is important that the dressing is comfortable for the patient, that dressing changes do not cause pain and the dressing does not restrict the patient’s daily activities (WCS Netherlands, 2020).
In general, wound assessment involves looking at: the location, size and depth of the wound, tissue colour, symptoms of infection, smell, amount of exudate, wound edges and surrounding skin (red, warm, softening, oedema) and the presence of pain (Zorg Voor Beter, 2023). Based on the assessment of these wound characteristics, an appropriate wound dressing can be chosen, taking into account the extent to which the characteristics of the wound dressing match the needs of the wound.
In this article, the focus is on a dressing spray, based on St John’s wort oil and neem oil (WOUND, Kerecis Switzerland), which is a hydro-active primary wound dressing spray that can be applied directly to the wound bed and surrounding skin; the spray creates a thin layer of oil (Figure 1) covering the wound bed (Eggenberger, 2013). The thin oil film prevents unwanted water evaporation from the wound, due to its hydrophobic nature.
Applying a non-adherent, indifferent secondary wound dressing (such as a non-adhesive absorbent dressing) after application of the spray additionally supports wound healing, as it prevents loss of the oil layer, absorption of moisture and damage to granulation tissue or regenerating epithelium during dressing changes.
The dressing spray also exerts an antimicrobial effect due to its high content of unsaturated fatty acids. The antimicrobial effects of unsaturated fatty acids, such as oleic acid and linoleic acid, are caused by their surface activity (electron chain disruption and oxidative phosphorylation) (Galbraith and Miller, 1973; Desbois and Smith, 2010). The periwound skin is often dry, scaly and irritated by wound exudate. Due to the high content of unsaturated fatty acids, the oil layer protects also the periwound skin and supports a healthy skin barrier function (Prottey et al, 1976). All these characteristics make the spray feasible for many wound types. Earlier case studies done by Mainetti and Carnevali (2013), Lenz (2015) and Luchli et al (2015) have already shown that the spray may have a beneficial effect on the wound-healing process.
In this case series, the aim was to evaluate the effects of this wound dressing spray on wound healing of acute (skin tears) and complex wounds (e.g. pressure ulcers) and to evaluate the feasibility of application and patient satisfaction with the spray.
Case series
In a Dutch nursing home (Breda, Noord-Brabant, Netherlands), residents with acute (skin tear) and ‘hard to heal’ wounds (pressure ulcers, venous leg ulcers, bullae) were screened for participation. Residents’ data and that of the wound healing process were collected from
the digital resident files. Next to this data, pain was measured using a 10-point Visual Analogue Scale (VAS-score):
- 1 = no pain
- 10 = most severe pain.
Comfort during wound treatment was assessed with a five-point Likert scale, which was also used by the nursing staff to rate the application process at the end of the period:
- 1 = very dissatisfied
- 2 = dissatisfied
- 3 = slightly satisfied
- 4 = satisfied
- 5 = very satisfied.
WOUND spray was applied by the nursing staff once per day from a distance of 5–10cm, directly into the wound bed and on the surrounding skin, until a clear oil layer was visible over the entire wound region. For residents who left the nursing home for one or more days (such as for home visits), the informal caregiver was also instructed to apply the spray. Two to three minutes after the formation of the oil layer, the total wound region was covered with an absorbent dressing.
Case study 1
This case concerns a 92-year-old female, admitted to the nursing home due to mobility impairment (caused by age) and venous insufficiency, for which the resident wears compression stockings. The venous insufficiency therapy also caused a severe hyperhidrosis of the leg and foot. The resident was wearing semi-orthopaedic footwear due to mobility impairment. Wearing the wrong new footwear caused a category III pressure ulcer on the instep of the foot. The wound size was: length 3.5cm, width 1.5cm and depth 0.5cm. The resident complained about a lot of pain (VAS-score 8/10).
The wound was initially treated in accordance with the protocol of the nursing home by applying full pressure relief and covering with a foam bandage. Initially, after the wound occurred, there was a sign of a possible infection (increase in wound fluid production, a lot of pain, stagnation of healing). In the first week a scab formed that came off after 10 days. At that moment a wound and an increase in fluid production was noticed. Measurement at day 10 showed no healing tendencies. The wound bed showed a yellow slough (60%), 40% red tissue and the wound edges were covered with callous. After debridement with a Debrisoft® pad, there was a switch from a foam dressing to WOUND spray 1xdd applied on the wound bed and surrounding skin (Figure 2A). Thereafter, the wound area was covered with Novopad® (a non-adhesive light absorbent compress with a polyethylene layer on both sides), which was fixed by an island plaster. The exudate production and the pain decreased rapidly in the first 2 days (VAS-score from 7/10 to 2/10). After 1 week, the wound had healed and treatment with WOUND was discontinued (Figure 2B).
Eight days after stopping using the spray the small crust spontaneously let go. The resident reported that the treatment with the spray was comfortable (comfort scale 5/5) and painless (VAS-score 1/10). Only a slight nasty smell after spraying, which disappeared quickly, was mentioned. The use of the spray, assessed by the nursing staff, scored 5/5 at the Likert scale.
Case study 2
This case concerns an 87-year-old female, admitted to the nursing home due to progressive dementia. She had a moderate mobility due to osteoarthritis of hips, knees and feet. Due to osteoarthritis of her feet the resident was wearing semi-orthopaedic footwear.
After a few days of wearing new footwear, a pressure ulcer on the left hallux of the big toe was visible. Initially, it was manifesting itself as a transparent blister (category II pressure ulcer). To protect the blister, pressure relief (no footwear) was realised and the blister was covered with a foam bandage. During the weekend the resident complained about increasing pain (VAS-score from 3/10 to 8/10) and redness and swelling of the forefoot occurred. Initially local treatment was continued in combination with antibiotic treatment and morphine, agreed by the physician on duty.
At assessment after the weekend (day six), a taut opaque blister was visible. The blister roof was removed and a small amount of debris was removed with a debridement pad. The measures of the wound bottom were: length 5cm, width 3cm and depth 0.1cm. Due to possible infection, WOUND spray 1xdd was started and covered with an absorbing bandage (Figure 3A/3B). After one week of treatment the wound showed a significant improvement. After two weeks a complete skin closure was realised (Figure 3C). Due to severe skin flaking in the surrounding area, intensive treatment with emollients were complementary to the wound treatment used.
Initially, the resident was very anxious about the wound treatment, but that disappeared after a few days. At the end of the treatment the VAS score was 1/10 and the wound treatment comfort score 4/5. The use of the spray, assessed by the nursing staff, scored 5/5 at the Likert scale for easy use.
Case study 3
A 95-year-old female was admitted to the nursing home due to a complicated hip fracture in combination with osteoarthritis. A head and neck prothesis, placed for the fracture, was loosened, but re-operation was not possible anymore. Additionally, the resident had venous insufficiency. Unfortunately, the resident refused to wear compression stockings/bandages. For walking inside the nursing home, she used a walker, for outside, a wheelchair.
Caused by a twisted left knee while walking, a knee tendon rupture and two skin tears arose on the left lower leg of type 2b (a skin tear where the edges cannot be realigned to the normal anatomical position and the skin or flap colour is pale, dusky or darkened; LeBlanc et al, 2016). The upper skin tear category II was 4cm long and 3.8cm width, the lower one was 7.5cm long and 6.5cm width. Treatment started in accordance with the protocol of the nursing home with a silicone gauze covered with an absorbing bandage; after three weeks the two skin tears showed no healing tendency and there was a lot of wound exudate, partly leaking oedema, partly wound exudate. Treatment was changed to spraying WOUND once a day, covered with an absorbing bandage and compressive bandaging
(Figure 4A). After two weeks, one skin tear was fully closed and after three weeks the other skin tear had healed (Figure 4B/4C).
Because the resident left the nursing home for three days, an informal caregiver changed the wound dressing during this time without any problems.
The resident only complained about the unpleasant smell of the spray, but found dressing changes quick and easy (comfort score 4/5) and painless (VAS-score 1/10). The nursing staff was also pleased with the change to the dressing spray (comfort Likert scale 5/5).
Case study 4
A 93-year-old female has lived for several years in the nursing home. She was admitted because she was not able to stay at home alone, was unable to walk more than three metres and used a wheelchair for mobility. She was known with a hypothyroidy and venous insufficiency in both legs following thrombosis. Because her skin was too vulnerable for compressive stockings, compression bandages were part of daily care. Soon after admission to the home, a bullous condition (possibly bullous pemphigoid) developed on her left lower leg. After unsuccessful treatment in the nursing home, the resident was under dermatologist treatment for four years without success. Various treatments were used without success: foam, alginate, silicone bandage, Suprasorb X+PMBH® and zinc oxide paste. Compressive bandages were continued. The local treatment was combined with dexamethasone in the six weeks before implementation.
Because there was no healing tendency the wound was divided in two halves: the upper part (approximately 10cm) was treated with silicone bandage and the lower part (approximately 10cm) with WOUND spray (day one) (Figure 5A). Both were covered with absorbing bandages and compressive bandages were continued. After 2 weeks, the lower half was almost fully epithelised (still a few small defects and a lot of dried spray oils were visible) (Figure 5B). Given the effect of treatment on the lower part, it was decided to treat the entire wound with WOUND. After 62 days, no more skin defects were visible, but still there were crusts remaining of dried spray (Figure 5C). These were not removed because of fear of damaging the vulnerable skin. The crusts spontaneously released in a period of 2 weeks and a healthy skin was visible.
Pain experience (VAS-score 2/10) did not change during the treatment period. The resident was very pleased with the application of the dressing spray, except for the smell, hence a 4/5 was scored at the comfort scale. The nursing staff scored on this scale also 4/5.
General conclusions of the nursing staff
After stopping the use of WOUND spray, nursing staff were asked their opinion of this wound treatment. The healthcare staff scored the spray an average of 4.5 out of 5 on the Likert scale for satisfaction and ease of applicability. The caregivers also indicated that when changing dressings, the absorbent bandage had to be wet only once before it could be removed. In addition, it also turned out to be easy and safe to have the treatment carried out by a caregiver after a short instruction if the resident was absent for more than a day.
Conclusion
This small case series shows that WOUND spray could be used for treatment of the chosen different types of wounds (one acute/traumatic and three complex wounds). The results show a tendency of positive effects (healing and no adverse events) and, except some complaints about smell, no other complaints have been noticed. The results are in agreement with the results of Mainetti and Carnevali (2013), Luchli et al (2014) and Lenz (2015). However, the study is too small to draw hard conclusions from it.
The simple method of application, which can also be carried out after a short instruction by informal caregivers, was highly appreciated by the professional and non-professional carers. The daily treatment also allowed a quick, non-time-consuming daily assessment of the wounds, which in case of insufficient efficacy, may lead to adjustment of the wound treatment. In this case series, no adjustment in wound treatment was necessary. Treatment did not need to change.
In conclusion, WOUND seems to be applicable to several types of wounds. Due to the simplicity of the treatment, this product can also be applied by non-care professionals. These positive results call for a larger, longitudinal randomised trial to further investigate, support and confirm them.
Conflict of interest
Participants and researcher did not receive any financial support. For all cases, WOUND spray was supplied free of charge by the manufacturer.
Introduction
Wound dressings play an important role in local wound care and contribute to achieving an antimicrobial environment where necessary, a balanced moist wound bed and protection of the periwound skin (Winter, 1962; Butcher, 2000; Cutting and White, 2002; Sharman, 2003; Burton, 2004; Cameron, 2004; Guo and DiPietro, 2010). It is important that the dressing is comfortable for the patient, that dressing changes do not cause pain and the dressing does not restrict the patient’s daily activities (WCS Netherlands, 2020).
In general, wound assessment involves looking at: the location, size and depth of the wound, tissue colour, symptoms of infection, smell, amount of exudate, wound edges and surrounding skin (red, warm, softening, oedema) and the presence of pain (Zorg Voor Beter, 2023). Based on the assessment of these wound characteristics, an appropriate wound dressing can be chosen, taking into account the extent to which the characteristics of the wound dressing match the needs of the wound.
In this article, the focus is on a dressing spray, based on St John’s wort oil and neem oil (WOUND, Kerecis Switzerland), which is a hydro-active primary wound dressing spray that can be applied directly to the wound bed and surrounding skin; the spray creates a thin layer of oil (Figure 1) covering the wound bed (Eggenberger, 2013). The thin oil film prevents unwanted water evaporation from the wound, due to its hydrophobic nature.
Applying a non-adherent, indifferent secondary wound dressing (such as a non-adhesive absorbent dressing) after application of the spray additionally supports wound healing, as it prevents loss of the oil layer, absorption of moisture and damage to granulation tissue or regenerating epithelium during dressing changes.
The dressing spray also exerts an antimicrobial effect due to its high content of unsaturated fatty acids. The antimicrobial effects of unsaturated fatty acids, such as oleic acid and linoleic acid, are caused by their surface activity (electron chain disruption and oxidative phosphorylation) (Galbraith and Miller, 1973; Desbois and Smith, 2010). The periwound skin is often dry, scaly and irritated by wound exudate. Due to the high content of unsaturated fatty acids, the oil layer protects also the periwound skin and supports a healthy skin barrier function (Prottey et al, 1976). All these characteristics make the spray feasible for many wound types. Earlier case studies done by Mainetti and Carnevali (2013), Lenz (2015) and Luchli et al (2015) have already shown that the spray may have a beneficial effect on the wound-healing process.
In this case series, the aim was to evaluate the effects of this wound dressing spray on wound healing of acute (skin tears) and complex wounds (e.g. pressure ulcers) and to evaluate the feasibility of application and patient satisfaction with the spray.
Case series
In a Dutch nursing home (Breda, Noord-Brabant, Netherlands), residents with acute (skin tear) and ‘hard to heal’ wounds (pressure ulcers, venous leg ulcers, bullae) were screened for participation. Residents’ data and that of the wound healing process were collected from
the digital resident files. Next to this data, pain was measured using a 10-point Visual Analogue Scale (VAS-score):
- 1 = no pain
- 10 = most severe pain).
Comfort during wound treatment was assessed with a five-point Likert scale, which was also used by the nursing staff to rate the application process at the end of the period:
- 1 = very dissatisfied
- 2 = dissatisfied
- 3 = slightly satisfied
- 4 = satisfied
- 5 = very satisfied).
WOUND spray was applied by the nursing staff once per day from a distance of 5–10cm, directly into the wound bed and on the surrounding skin, until a clear oil layer was visible over the entire wound region. For residents who left the nursing home for one or more days (such as for home visits), the informal caregiver was also instructed to apply the spray. Two to three minutes after the formation of the oil layer, the total wound region was covered with an absorbent dressing.
Case study 1
This case concerns a 92-year-old female, admitted to the nursing home due to mobility impairment (caused by age) and venous insufficiency, for which the resident wears compression stockings. The venous insufficiency therapy also caused a severe hyperhidrosis of the leg and foot. The resident was wearing semi-orthopaedic footwear due to mobility impairment. Wearing the wrong new footwear caused a category III pressure ulcer on the instep of the foot. The wound size was: length 3.5cm, width 1.5cm and depth 0.5cm. The resident complained about a lot of pain (VAS-score 8/10).
The wound was initially treated in accordance with the protocol of the nursing home by applying full pressure relief and covering with a foam bandage. Initially, after the wound occurred, there was a sign of a possible infection (increase in wound fluid production, a lot of pain, stagnation of healing). In the first week a scab formed that came off after 10 days. At that moment a wound and an increase in fluid production was noticed. Measurement at day 10 showed no healing tendencies. The wound bed showed a yellow slough (60%), 40% red tissue and the wound edges were covered with callous.
After debridement with a Debrisoft® pad, there was a switch from a foam dressing to WOUND spray 1xdd applied on the wound bed and surrounding skin (Figure 2A). Thereafter, the wound area was covered with Novopad® (a non-adhesive light absorbent compress with a polyethylene layer on both sides), which was fixed by an island plaster. The exudate production and the pain decreased rapidly in the first 2 days (VAS-score from 7/10 to 2/10). After 1 week, the wound had healed and treatment with WOUND was discontinued (Figure 2B).
Eight days after stopping using the spray the small crust spontaneously let go. The resident reported that the treatment with the spray was comfortable (comfort scale 5/5) and painless (VAS-score 1/10). Only a slight nasty smell after spraying, which disappeared quickly, was mentioned. The use of the spray, assessed by the nursing staff, scored 5/5 at the Likert scale.
Case study 2
This case concerns an 87-year-old female, admitted to the nursing home due to progressive dementia. She had a moderate mobility due to osteoarthritis of hips, knees and feet. Due to osteoarthritis of her feet the resident was wearing semi-orthopaedic footwear.
After a few days of wearing new footwear, a pressure ulcer on the left hallux of the big toe was visible. Initially, it was manifesting itself as a transparent blister (category II pressure ulcer). To protect the blister, pressure relief (no footwear) was realised and the blister was covered with a foam bandage. During the weekend the resident complained about increasing pain (VAS-score from 3/10 to 8/10) and redness and swelling of the forefoot occurred. Initially local treatment was continued in combination with antibiotic treatment and morphine, agreed by the physician on duty.
At assessment after the weekend (day six), a taut opaque blister was visible. The blister roof was removed and a small amount of debris was removed with a debridement pad. The measures of the wound bottom were: length 5cm, width 3cm and depth 0.1cm. Due to possible infection, WOUND spray 1xdd was started and covered with an absorbing bandage (Figure 3A/3B). After one week of treatment the wound showed a significant improvement. After two weeks a complete skin closure was realised (Figure 3C). Due to severe skin flaking in the surrounding area, intensive treatment with emollients were complementary to the wound treatment used.
Initially, the resident was very anxious about the wound treatment, but that disappeared after a few days. At the end of the treatment the VAS score was 1/10 and the wound treatment comfort score 4/5. The use of the spray, assessed by the nursing staff, scored 5/5 at the Likert scale for easy use.
Case study 3
A 95-year-old female was admitted to the nursing home due to a complicated hip fracture in combination with osteoarthritis. A head and neck prothesis, placed for the fracture, was loosened, but re-operation was not possible anymore. Additionally, the resident had venous insufficiency. Unfortunately, the resident refused to wear compression stockings/bandages. For walking inside the nursing home, she used a walker, for outside, a wheelchair.
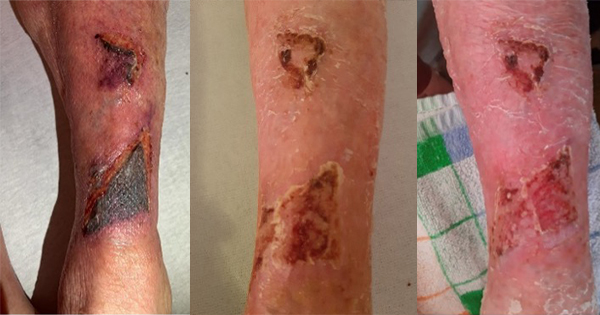
Caused by a twisted left knee while walking, a knee tendon rupture and two skin tears arose on the left lower leg of type 2b (a skin tear where the edges cannot be realigned to the normal anatomical position and the skin or flap colour is pale, dusky or darkened; LeBlanc et al, 2016). The upper skin tear category II was 4cm long and 3.8cm width, the lower one was 7.5cm long and 6.5cm width. Treatment started in accordance with the protocol of the nursing home with a silicone gauze covered with an absorbing bandage; after three weeks the two skin tears showed no healing tendency and there was a lot of wound exudate, partly leaking oedema, partly wound exudate. Treatment was changed to spraying WOUND once a day, covered with an absorbing bandage and compressive bandaging
(Figure 4A). After two weeks, one skin tear was fully closed and after three weeks the other skin tear had healed (Figure 4B/4C).
Because the resident left the nursing home for three days, an informal caregiver changed the wound dressing during this time without any problems.
The resident only complained about the unpleasant smell of the spray, but found dressing changes quick and easy (comfort score 4/5) and painless (VAS-score 1/10). The nursing staff was also pleased with the change to the dressing spray (comfort Likert scale 5/5).
Case study 4
A 93-year-old female has lived for several years in the nursing home. She was admitted because she was not able to stay at home alone, was unable to walk more than three metres and used a wheelchair for mobility. She was known with a hypothyroidy and venous insufficiency in both legs following thrombosis. Because her skin was too vulnerable for compressive stockings, compression bandages were part of daily care. Soon after admission to the home, a bullous condition (possibly bullous pemphigoid) developed on her left lower leg. After unsuccessful treatment in the nursing home, the resident was under dermatologist treatment for four years without success. Various treatments were used without success: foam, alginate, silicone bandage, Suprasorb X+PMBH® and zinc oxide paste. Compressive bandages were continued. The local treatment was combined with dexamethasone in the six weeks before implementation.
Because there was no healing tendency the wound was divided in two halves: the upper part (approximately 10cm) was treated with silicone bandage and the lower part (approximately 10cm) with WOUND spray (day one) (Figure 5A). Both were covered with absorbing bandages and compressive bandages were continued. After 2 weeks, the lower half was almost fully epithelised (still a few small defects and a lot of dried spray oils were visible) (Figure 5B). Given the effect of treatment on the lower part, it was decided to treat the entire wound with WOUND. After 62 days, no more skin defects were visible, but still there were crusts remaining of dried spray (Figure 5C). These were not removed because of fear of damaging the vulnerable skin. The crusts spontaneously released in a period of 2 weeks and a healthy skin was visible.
Pain experience (VAS-score 2/10) did not change during the treatment period. The resident was very pleased with the application of the dressing spray, except for the smell, hence a 4/5 was scored at the comfort scale. The nursing staff scored on this scale also 4/5.
General conclusions of the nursing staff
After stopping the use of WOUND spray, nursing staff were asked their opinion of this wound treatment. The healthcare staff scored the spray an average of 4.5 out of 5 on the Likert scale for satisfaction and ease of applicability. The caregivers also indicated that when changing dressings, the absorbent bandage had to be wet only once before it could be removed. In addition, it also turned out to be easy and safe to have the treatment carried out by a caregiver after a short instruction if the resident was absent for more than a day.
Conclusion
This small case series shows that WOUND spray could be used for treatment of the chosen different types of wounds (1 acute/traumatic and 3 complex wounds). The results show a tendency of positive effects (healing and no adverse events) and, except some complaints about smell, no other complaints have been noticed. The results are in agreement with the results of Mainetti and Carnevali (2013), Luchli et al (2014) and Lenz (2015). However, the study is too small to draw hard conclusions from it.
The simple method of application, which can also be carried out after a short instruction by informal caregivers, was highly appreciated by the professional and non-professional carers. The daily treatment also allowed a quick, non-time-consuming daily assessment of the wounds, which in case of insufficient efficacy, may lead to adjustment of the wound treatment. In this case series, no adjustment in wound treatment was necessary. Treatment did not need to change.
In conclusion, WOUND seems to be applicable to several types of wounds. Due to the simplicity of the treatment, this product can also be applied by non-care professionals. These positive results call for a larger, longitudinal randomised trial to further investigate, support and confirm them.
Conflict of interest
Participants and researcher did not receive any financial support. For all cases, WOUND spray was supplied free of charge by the manufacturer