Chronic wounds have been defined as wounds that fail to progress in an orderly and timely manner to restore the anatomic and functional integrity of the injured site (Shivani et al, 2021). Those chronic wounds have a clear underlying cause and are largely assigned to leg ulcers (frequently a consequence of venous or arterial deficiencies — venous or arterial leg ulcers), diabetic foot ulcers, or pressure injuries (Nunan et al, 2014). It is stated that appropriately identifying the aetiology of a chronic wound and the local and systemic factors that may be cause of delayed or stalled wound healing, is crucial to successful wound management (Pant et al, 2019).
These wounds represent a significant health concern to both clinicians and patients, posing both a financial and psychological impact, and managing these patients represents a high cost in terms of both time and resources required (Järbrink et al, 2017).
It is estimated that globally, chronic wounds of mixed aetiologies represent a prevalence of 2.21 per 1,000 population, and for leg ulcers, the prevalence is estimated at 1.51 per 1,000 (Martinengo et al, 2019). However, there seems to be a lack of studies regarding the epidemiology in India, with one study (Gupta et al, 2004), putting the prevalence of chronic wounds in the community as 4.5 per 1,000 population.
Moreover, infections in wound management are closely associated with delayed healing, increased complications, such as amputation, as well as increasing the negative impact on patients’ quality of life (Cutting et al, 2016; Armstrong et al, 2017). Due to the complications that ensue, infections also increase the economic burden on healthcare facilities related to wound management and increase in hospital stay (Nussbaum et al, 2018). Management of wound infection includes understanding and involvement of the patient’s response, the local wound-healing environment, and a reduction of the microbial load as part of the standard of care, including wound cleansing, debridement, and appropriate use of topical antimicrobials (International Wound Infection Institute [IWII], 2022).
Additionally, the presence of nonviable tissue plays a prominent role in chronicity — eschar and slough provide an optimal environment for the multiplication of microorganisms that prolong the inflammatory phase of healing and can act as a reservoir for biofilms (Percival and Suleman, 2015). Biofilms stimulate an inflammatory response, increasing vascular permeability, oedema and exudate production, which may be interconnected with slough production (Dowd et al, 2008). Desloughing of wounds is, therefore, a critical component of the wound bed preparation to facilitate healing (Vowden and Vowden, 2011). While the removal of eschar is usually achieved by sharp and surgical debridement, desloughing is more often attained by conservative methods, including the use of local dressings that promote autolysis and safe mechanical methods (Grothier, 2015). Modern approaches, such as autolytic debridement with polyacrylate fibre dressings, offer a safe and effective method to remove this debris from the wound bed (Milne, 2015).
Poly-absorbent fibres impregnated with a silver lipido-colloid matrix
Poly-absorbent fibres have been shown to be effective in desloughing — this was portrayed in a randomised controlled trial (RCT) (Meaume et al, 2014), where the poly-absorbent fibres showed similar efficacy and safety when compared with Hydrofiber but presented significantly better desloughing properties in the management of ulcers.
Silver lipido-colloid matrix has also been recognised in its effectiveness in the management of wounds presenting three of five clinical signs of local infection by means of two RCTs (Harding et al, 2012; Lazareth et al, 2012). Poly-absorbent fibre impregnated with a silver lipido-colloid matrix dressing addresses the high microbial burden that can delay or prevent wound healing, as well as being effective against biofilms (Desroche et al, 2016).
In vitro studies show its broad-spectrum antimicrobial capability, including Staphylococcus aureus, Pseudomonas aeruginosa, vancomycin-resistant Enterococci and methicillin-resistant Staphylococcus aureus (MRSA) (Desroche et al, 2016), and significant reduction of biofilm volume, disrupting the integrity of the biofilm after 24 hours of exposure (Percival et al, 2012).
In a non-comparative RCT (Dalac et al, 2016) including 37 patients with chronic wounds mostly covered by sloughy tissue, the average wound area was reduced by 32.5% within a maximum of 4 weeks treatment, the clinical score (maximum value of five, based on inflammatory clinical signs) decreased from 4.0 to 2.0, while also effective debridement properties were documented (62.5% relative reduction of sloughy tissue at week four and 58.8% of debrided wounds at week four).
A large, prospective, multicentre, real-life observational study was conducted in 81 centres in Germany involving 2,270 patients, to evaluate the poly-absorbent fibre impregnated with a silver lipido-colloid matrix dressing, to determine, the short-term clinical impact of the dressing on the wound-healing process (Dissemond et al, 2020). The patients included in the study had both acute and chronic wounds of various aetiologies that were treated with the dressing for a mean duration of 22±13 days. The authors stated that all clinical signs of local infection and the diagnosed wound infections were substantially reduced by 2 weeks after the treatment initiation, while all wound infection clinical signs continued to reduce until the last visit.
Additionally, clinical improvement in wound healing was reported in 98.9% of acute wounds, with a wound closure rate of 68.5%, and, in chronic wounds, a median RWAR (Relative Wound Area Reduction) of 57.4% was achieved. An improvement in healing process was noted by clinicians in 90.6% of cases and stabilisation in 6.1%, regardless of exudate level and proportion of slough and granulation tissue in the wound bed at baseline.
In view of this evidence, the authors wanted to evaluate the clinical outcomes of using the poly-absorbent fibres impregnated with a silver lipido-colloid matrix in the management of chronic wounds in patients hailing from different areas of India.
Case 1
Anoop Vasudevan Pillai, MS. Assistant Professor, Department of General Surgery, Amrita Institute of Medical Sciences, Kochi, Kerala.
Riju R Menon, DNB, Professor, Department of General Surgery, Amrita Institute of Medical Sciences, Kochi, Kerala.
This case centres on a 67-year-old housewife with diabetes, who had undergone a known post-great toe amputation, presented with right infected DFU with abscess in the plantar aspect of foot. The abscess had partially ruptured spontaneously prior to arrival at our hospital. Drainage of the abscess and debridement of the local area was conducted under ankle block. The ulcer was 15 x 9cm ulcer with profuse slough (70%), exposed tendons, and necrotic tissue (10%) in the wound bed. It was highly exudative, with oedema and necrosis of the margin of the ulcer [Figure 1]. The wound was described by the patient as painful (Visual Analogue Scale — VAS (Brazier et al 2017] of 6–7). A tissue culture was obtained, and parenteral and Cefoperazone-sulbactam (1.5gm IV q12H) antibiotics initiated.
The poly-absorbent fibres impregnated with a silver lipido-colloid matrix dressing was initiated as the primary dressing, with dressing changes every five days. At 2 weeks, wound size minimally reduced (14 x 9cm) [Figure 2]. Slough tissue was reduced to 30%, and necrotic to 5%, with healthy granulation tissue covering most of the wound bed. Pain score was also reduced to VAS 4. By the sixth week, wound size reduced considerably, without any slough [Figure 3]. Pain was minimal (VAS 2). Dressings were being changed every 5 to 7 days. Although tendon at the centre of the wound was still visible, granulation was noted to be better than the previous dressing changes. By the tenth week the wound had contracted nearly 90%, with healthy supple scar noted in the upper and lower aspects of the wound, and wound bed filled with healthy granulation tissue [Figure 4]. Previously macerated edges were also resolved.
Although the Department of General Surgery Amrita institute of Medical Sciences, Kochi considers a variety of dressing materials and innovations for wound healing, the Poly-absorbent fibres impregnated with a silver lipido-colloid matrix dressing is used in our daily practice in selected patients with excellent results.
Since this patient had a very complicated DFU with abscess and major comorbidities, there was a risk of limb loss. Hence, the clinician opted for a dressing that would address slough removal, promote healing, and require fewer dressings, which would be cost-effective.
It was concluded that, in this case, poly-absorbent fibres impregnated with a silver lipido-colloid matrix dressing accelerated the healing process and helped in removing slough and biofilms, as well as promoted granulation tissue formation and gave a supple cosmetic scar. It is also suggested that dressings changed once every 5 days is cost effective. Moreover, the dressings are patient-friendly with reduction in pain scores.
Case 2
KVNN Santosh Murthy, MS. General Surgery, Consultant General, Podiatric & Burns Surgeon; Founder of Advanced Wound Healing Clinics, Nalgonda Town, Telangana state
A 52-year-old female, know case of diabetes mellitus and peripheral arterial disease, presented with a 15 x 7 x 3cm infected, sloughy wound on the plantar aspect of the left foot [Figure 5]. Surgical debridement was conducted, and Poly-absorbent fibres impregnated with a silver lipido-colloid matrix dressing was initiated as the primary dressing.
The wound progressed well with the treatment, and, within three weeks, there was a significant reduction in slough, gradual improvement of granulation tissues and complete removal of necrotic tissues [Figure 6]. By week five, the wound continued to progress with further reduction of non-viable tissue [Figure 7] and on the sixth week, the wound was totally covered with healthy granulation tissue [Figure 8]. By the seventh week, a session of negative pressure wound therapy was conducted and finally the wound was grafted [Figure 9], and the wound was considered as completely healed by week 10 [Figure 10].
With the treatment of poly-absorbent fibres impregnated with a silver lipido-colloid matrix dressing, the wound size reduced, wound bed improved, exudate level reduced and signs of local infection were eliminated, which allowed the graft procedure. In addition, there was a reduction in pain.
The clinician concluded that poly-absorbent fibres impregnated with a silver lipido-colloid matrix dressing is convincing and is recommended for sloughy wounds due to its desloughing and continuous cleaning properties, as well as exudate reduction that decreases the usage of many absorbent dressings and dressing change frequency. Moreover, the antimicrobial action was deemed effective in the management of the local wound infection.
Case 3
Divya Prakash, MS (General Surgery), MCh (Plastic Surgery), DNB (Plastic Surgery), Consultant Plastic Surgeon, Kauvery Hospital, Trichy.
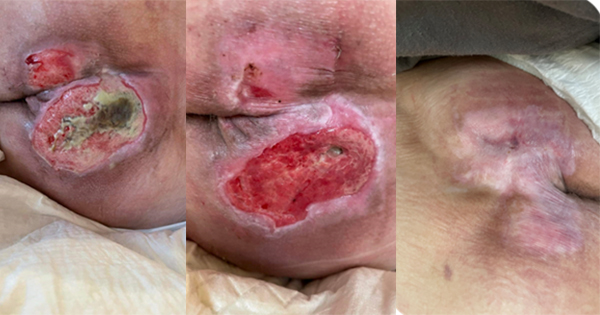
A 52-year-old gentleman has been living with type 2 diabetes mellitus for 10 years, non-compliant to medications. Patient presented with a 2-week history of blackish discolouration with sudden onset of blisters in right lower limb. On admission, the diagnosis was necrotising fasciitis. Surgical wound debridement was conducted, and intravenous antibiotics administered [Figure 11]. Poly-absorbent fibres impregnated with a silver lipido-colloid matrix dressing was started as the primary dressing. Dressings were initially changed on alternate day. Within 2 weeks of the treatment, the wound exudation and dressing soakage gradually reduced in response to the increasing healthy granulation [Figure 12]. Dressing changes were done every 3 days. By the fourth week, granulation started to bridge the exposed tibia bone [Figure 13] which was completely bridged by the sixth week [Figure 14]. The granulation tissue was deemed fit for grafting and a split-thickness graft was performed on day 39 [Figure 15]. The dressings prepared the wound bed tissue quite well to receive the graft, with no rejection of the graft thereafter.
The healing time was less than one and half month. The size of wound reduced by 8cm in length, slough replaced with healthy granulation and the exposed tibia eventually got bridged with healthy granulation in five and a half weeks from the start of treatment. Patient subjectively felt less pain and wound discharge after day 13.
The clinician was pondering for reconstructive options to cover the bone, or even of amputation options. However, within two weeks, the poly-absorbent fibres impregnated with a silver lipido-colloid matrix dressing started to produce healthy red granulation. It may be concluded that the dressing helped in preventing a major reconstructive surgery and the patient is now walking again. It was concluded that the poly-absorbent fibres impregnated with a silver lipido-colloid matrix dressing has potentially saved a limb, time, money and from challenging reconstructive procedures.
Case 4
Sangeetha Kalabhairav, MS. Diabetic Foot, Nail Surgeon and Podiatrist; Sushrutha Multi-speciality Hospital, Vidyanagar, Hubli.
A 65-year-old male patient with low socioeconomic background presented with non-healing ulcer over left leg that was present for one year, gradual in onset and progressive in nature with associated pruritis surrounding the ulcer and pain. The wound bed was covered with slough and unhealthy granulation tissue with moderate discharge and surrounding area was thick and hyperpigmented with tenderness [Figure 16]. The patient rated wound pain as severe (VAS 7). Oral empirical antibiotics were started (oral Clindamycin 300mgs. Eight hourly for 7 days after culture results). The wound was cleansed with wound cleansing spray and debridement carried out at the out-patient department. Poly-absorbent fibres impregnated with a silver lipido-colloid matrix dressing was applied on the wound under four-layer compression bandage.
The dressing was changed every three to four days initially and later frequency of dressing reduced to once every 6 days. After 2 weeks of treatment, the wound had reduced in size, measuring 10cm (length) x 5cm (width) x 0.25cm (depth) [Figure 17], and wound continued to reduce in size by week three. Slough had completely disappeared, wound bed appeared healthy with granulating tissue and the patient reported moderate pain (VAS 4). Progress in the wound continued to be noted by the third week [Figure 18]. Within 5 weeks the wound bed surface area reduced to 2cm by 2cm [Figure 19].
In this case, the clinician noted reduction in oedema, malodour, maceration, wound-related pain and rapid wound bed improvement and wound area reduction. It was concluded that Poly-absorbent fibres impregnated with a silver lipido-colloid matrix dressing is effective in the management of the venous leg ulcer along with four-layer compression bandage, suggesting that the dressing is advantageous for managing venous ulcers. The dressing was considered beneficial as the amount of peri-wound maceration appears to be less in comparison to other treatments, mainly due to its gel forming technology. Due to its properties, including desloughing, good absorption of exudate, granulation tissue formation, promotion of the healing process (reduction in area) of ulcer, the clinician considers the poly-absorbent fibres impregnated with a silver lipido-colloid matrix dressing a cost-effective option that increases good patient compliance. The dressing was also reported as easy to apply with pain free removal. This is beneficial for community carers to apply the treatment with ease.
Case 5
Anshumali Misra, DNB, MCh, Senior Consultant Plastic Microvascular and Cosmetic Surgery Max Hospital, New Delhi.
A 45-year-old male, known diabetes mellitus on intermittent treatment, was admitted in a local hospital with two large ulcers on the left lower limb (almost entire anterior-lateral aspect, extending posteriorly [Figure 20]. The wound was previously managed with gauze and povidone-iodine. Multiple sessions of radical surgical debridement in operating room debridement were conducted.
On presentation the wound was 50% covered with slough. Post debridement a large wound of nearly 8 x 19 cm was created. Poly-absorbent fibres impregnated with a silver lipido-colloid matrix dressing was initiated as the primary dressing and within two weeks slough was reduced to 30%. Within 4 weeks of the treatment, the wound was showing good progress [Figure 21]. By the fifth week, one session of negative pressure wound therapy was conducted and the wound was finally grafted [Figure 22].
Within the total treatment of five weeks (four weeks of management with Poly-absorbent fibres impregnated with a silver lipido-colloid matrix dressing and 4 days of NPWT), the wound bed had been prepared for split thickness skin grafting. Slough was completely removed, and healthy granulation tissue achieved.
The clinician concluded that Poly-absorbent fibres impregnated with a silver lipido-colloid matrix dressing is a good alternative to prepare wound bed when wound presents with slough and infection as it offers the dual advantage of a non-adhesive absorbent dressing embedded with an effective antimicrobial. The dressing reduced the potential recurrence of infection possibly due to constant supply of an antimicrobial agent and the continuous cleaning.
Case 6
Bhavin Ram, MS. Consultant Vascular and Endovascular Surgeon, Yashoda Hospitals, Secunderabad, Hyderabad.
A 39-year-old male patient with diabetes presented with a 4-week history of a right leg non healing 9 x 6cm wound with mild purulent discharge on medial aspect of the right lower leg above the malleolus, with surrounding black pigmentation [Figure 23]. The wound was diagnosed as a venous ulcer. Right great saphenous vein endovenous ablation was performed in view of reflux at sapheno-femoral junction and wound management initiated with Poly-absorbent fibres impregnated with a silver lipido-colloid matrix dressing and four-layer compression bandaging.
Initially dressing changed every fourth day, and by the fourth dressing change, within two weeks, no purulent discharge was noted, and the wound appeared healthier [Figure 24]. By this time, pain was reduced from VAS 8 to VAS 3. The same management was continued, and the wound was completely healed within 4 weeks [Figure 25].
The clinician concluded that the Poly-absorbent fibres impregnated with a silver lipido-colloid matrix dressing should be considered for infected venous ulcer and associated risk factors causing increase in infection like in this case with underlying diabetes mellitus. It provides a synergistic effect with compression dressing thus alleviating fear of increasing local infection. The dressing is also ideal under compression, as it does not require frequent changes.
Conclusion
Wound infection has always been a challenge for clinicians and patients (Frykberg and Banks, 2015). Contemporary wound management should be based on evidence to ensure that patients are receiving safe and effective care (Welsh, 2018).
The six cases involving patients from different regions from India with chronic wounds discussed in this article were managed under real-life conditions. The outcomes, after the application of the poly-absorbent fibre impregnated with a silver lipido-colloid matrix dressing, in all the six cases are very encouraging, showing a rapid decrease of the inflammatory signs and of the slough tissue as complete healing in some cases and preparation of graft procedures in other cases. The results of these clinical cases are similar with the findings documented in real-life observational study (Dissemond et al, 2020a), supporting the use of this particular dressing for patients in India.