NPWT is one of a number of advanced interventions that clinicians consider when the use of passive dressings alone is deemed to be insufficient for the topical management of wounds. At the start of her presentation, Rosa Somma described NPWT as the topical application of negative (sub-atmospheric) pressure at the wound-dressing interface. Numerous NPWT systems are described in the literature but they all generally follow the same basic principles, i.e. (i) coverage/filling of a wound with a dressing, (ii) creation of a seal by applying an adhesive dressing or drape, (iii) application of negative pressure via tubes which connect the dressing to a pump and a canister for fluid collection (Norman et al, 2020).
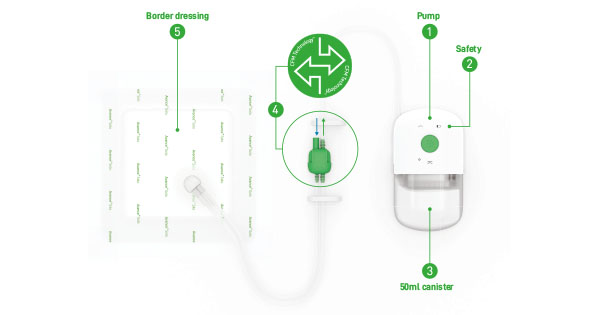
The ‘traditional’ NPWT systems are reliant on a mains electricity source which, when taken into consideration alongside their size and weight, has restricted their use to mainly acute care. However, the introduction of portable, single-use negative pressure wound therapy (suNPWT) systems that are typically lighter and smaller in size than their traditional counterparts and are powered mechanically or by batteries, has enabled this much-valued therapy to be accessible to a greater population of patients, such as those in post-acute and community care settings (Orlov and Gefen, 2022). The available suNPWT systems generally fall into one of two categories, i.e. whether they are supplied with a canister or otherwise. Canister-free systems rely solely on the dressings to manage exudate through absorption and evaporation. In contrast, the canister-based (CB) systems, such as Avance® Solo [Figure 1], incorporate a canister in their design, which enables exudate and infectious material to be continually removed from the dressing that is in contact with the wound (Henriksson, 2021).
Rosa went on to describe how NPWT causes two types of tissue deformation — macro-deformation (i.e. visible to the naked eye) and micro-deformation (i.e. at the microscopic level) [Figure 2]. She then focused on the wound-dressing interface, comparing a foam dressing typically used with a traditional NPWT system with the multi-layer dressing supplied with the Avance Solo NPWT system.
Rosa described how, with the traditional NPWT system, the application of pressure causes the dressing to displace into the wound cavity, resulting in a pressure differential between the margins (higher pressure) and centre (lower pressure) of the wound. This higher pressure has the potential to compress capillaries and create hypoperfusion which, in turn, inhibits cellular proliferation [Figure 3a]. In comparison, the structure of the multi-layer dressing supplied with Avance Solo is more resistant to the effects of the applied pressure and, thus, promotes a more even distribution of pressure across the wound without areas of hypoperfusion [Figure 3b]. While positive pressure and mechanical aggravation stimulate the formation of granulation tissue, mechanical traction and hypoperfusion inhibit cell proliferation and wound edge advancement.
Rosa then described her clinical experience using Avance Solo, a single-use NPWT system designed with a canister and featuring Controlled Fluid Management (CFM) Technology™. This technology secures continuous delivery of effective negative pressure therapy of –125 mmHg to the wound site. A controlled inflow of air through a filter placed in the ‘quick’ connector manages transportation of excess exudate from the dressing and it is collected in the canister. With CFM Technology™, the delivery of negative pressure is not compromised by fluid accumulation in the absorptive dressing — a shortcoming often associated with canisterless NPWT systems.
With the Avance Solo NPWT system, exudate and infectious material are managed by a combination of absorption in the multi-layer bordered dressing, and transportation of excess fluid to the canister, therefore reducing the risk of the dressing becoming saturated and interrupting the delivery of negative pressure to the wound (Henriksson, 2021; Orlov and Gefen, 2021).
Avance Solo is intended for use on a variety of surgical closed wounds, open wounds, grafts and flaps. The dressing is designed with Safetac® technology in both wound contact layer and borders, and the dressing can be combined with a foam wound filler for cavity wounds.
Cases using NPWT with and without a canister
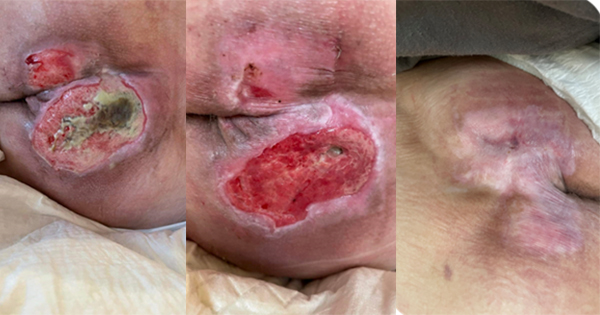
Rosa detailed a case where healing of a wound had been delayed by 3 to 4 weeks after the use of a system without a canister. The system was unable to correctly manage the exudate and resulted in maceration of the periwound skin and compromised the healing process. Following an ultrasound debridement, the use of Avance Solo resolved the damage in 10 days. The patient then underwent a skin graft but, again, a system without a canister damaged the skin graft [Figure 4].
Managing exudate and stimulating perfusion are important and the inclusion of a canister in the Avance Solo system enables exudate and infectious material to be continually removed from the dressing that is in contact with the wound. In the absence of a canister, the dressings used in conjunction with canisterless systems are only able to manage exudate by absorption and evaporation (Henriksson, 2021).
In the final part of her presentation, Rosa described how a small pilot study (5 patients) had been undertaken to evaluate the ability of Avance Solo to manage exudate and stimulate perfusion of wounds of various aetiology. NPWT was used for a 4-week period, with weekly dressing changes. Dressings were weighed before application and after removal in order to measure exudate quantity. Laser photography was used to measure wound size and micro-circulation in the wound bed was assessed by laser doppler imaging. The case presented in Figure 5 is typical of the outcomes observed for all patients.
Dehiscence prevention with NPWT: The reality in cardiothoracic surgery
Viviana Gonçalves outlined the work conducted at her Cardiothoracic Surgery Department, which is the biggest such department in Portugal and carries out approximately 1,600 cardiac surgeries per year. Before each surgery, the patient undergoes a consultation to address modifiable and non-modifiable risk factors for surgical wound complications and dehiscence. Preventative and risk-reduction measures are taken where possible before the surgery.
Surgical wound dehiscence is the separation of the margins of a closed surgical incision, with or without exposure or protrusion of underlying tissue, organs or implants (Sandy-Hodgetts, 2018). It tends to be more common in patients classed as high-risk with comorbidities such as diabetes, peripheral vascular disease or obesity, as well as those who have undergone multiple surgeries with time gaps. Female patients are found to be at a higher risk of dehiscence.
NPWT has been shown to lower the incidence of dehiscence and infection in post-surgical wounds (Stannard et al, 2012; Wounds UK, 2013), and it is often used in the management of complex wounds where wound healing is particularly challenging. NPWT at -125mmHg as a preventative measure has also been found to have a good cost-benefit ratio, as well as better scarring outcomes.
Viviana talked through some patient case studies, which showed some positive results using NPWT after heart surgeries (see Box 1 for summarised case studies).
Case study evaluations of NPWT on open wounds
The Avance Solo system can be used in a variety of wound types, as seen in Table 1. Arja Korhonen introduced some recent case studies where NPWT was used with positive results on some complex open wounds (see Box 2 for summarised case studies).
Finally, Tiina Pöllänen presented two case studies in which the Avance Solo System was associated with successful management of both open surgical wounds and closed surgical incision sites [Box 3].
Conclusions
The application of NPWT has emerged as an effective means of reducing the risk of generally avoidable complications. The case studies shared in this symposium demonstrated its efficacy and safety in a wide range of clinical settings.
Historically, the use of NPWT was generally confined to acute care, mainly due to the size and weight of the systems and their dependence on a mains electricity source. The recent introduction of portable, single-use systems has now opened up NPWT to hospital outpatients and those being cared for in the community, including ambulatory patients.
With the Avance Solo NPWT system, exudate and infectious material are managed by a combination of absorption in the multi-layer bordered dressing and transportation of excess fluid to the canister, therefore reducing the risk of the dressing becoming saturated and interrupting the delivery of negative pressure to the wound (Davies, 2022).
The cases presented by the speakers on the use of Avance Solo in practice demonstrated accelerated and effective healing in a variety of wound types.