This case study outlines the establishment of lymphoedema services at Nantucket Cottage Hospital (NCH), part of the Mass General Brigham system, located in Nantucket (MA, USA), addressing the unique challenges posed by geographic isolation. Over 20 patients benefited from improved access to care in 2024, with high levels of patient satisfaction reported. The findings underscore the importance of specialized management in enhancing patient outcomes in remote areas. Specific patient demographics, treatment modalities, and care strategies are discussed, with comparisons to national trends and the impact of the service on the island community.
Introduction
Lymphoedema, a chronic condition marked by the accumulation of lymphatic fluid leading to swelling, significantly impacts patients’ health and quality of life if left untreated. Effective management requires comprehensive interventions such as manual lymphatic drainage, compression therapy, exercise, patient education and skin care, all delivered by certified specialists. This condition is particularly prevalent among cancer survivors, with notable incidence rates linked to breast, gynaecological, and head and neck cancers. Factors influencing lymphoedema development include surgical interventions, radiation therapy, and patient-specific characteristics, such as obesity (Ryu et al, 2024).
Nantucket, with its unique geographical isolation and a population swelling from 14,445 to over 80,000 in summer, historically faced gaps in lymphoedema management. Until the establishment of local services in 2023, patients experienced delays seeking treatment on the mainland, resulting in poorer health outcomes and increased risk of complications. This gap underscored the critical importance of accessible, timely care, reflecting national and global findings that highlight the substantial impact of delayed treatment on lymphoedema prognosis (Ryu et al, 2024).
Prevalence estimates for secondary lymphoedema remain significant, affecting 1 in 1,000 Americans. The condition is particularly under-reported, with cancer treatments elevating the risk; up to 20% of breast cancer survivors and approximately 37% of women treated for gynaecological cancers develop measurable lymphoedema. These data reinforce the necessity for proactive lymphoedema management to mitigate both physical and psychosocial challenges (Ryu et al, 2024; Yoon et al, 2024).
This case study examines the implementation of lymphoedema services at NCH, detailing the challenges faced and solutions implemented to address the urgent healthcare needs of the community. It also compares patient demographics and trends to national averages to better understand the local impact.
Objectives
The objectives of this study are to:
- Document the challenges in providing lymphoedema services in a remote location.
- Evaluate the effectiveness of interdisciplinary collaboration.
- Provide recommendations for future service improvement.
Methods
The lymphoedema team at NCH consists of one certified lymphoedema therapist (CLT), an oncologist, nurses and primary care providers. Additionally, there is collaboration with off-island oncologists to ensure comprehensive patient care. Patients are initially assessed during a comprehensive evaluation, followed by treatment sessions, which occur 5 days a week for 3–4 weeks lasting 60–90 minutes. Ongoing education and support are provided throughout treatment. The CLT also received mentorship from certified lymphoedema therapists at Massachusetts General Hospital and Beth Israel Deaconess Medical Center, which proved invaluable given the remote setting and lack of local resources.
Results
In its first year, NCH’s lymphoedema service treated over 20 patients. The patient population consisted of both year-round locals and seasonal residents, with a predominance of female patients. Most presented with secondary lymphoedema in the arms and legs due to cancer treatments, particularly breast and gynaecological cancers. The service was offered year-round, with a notable influx of patients during the summer months when the population swells, leading to a need for temporary expansion of services.
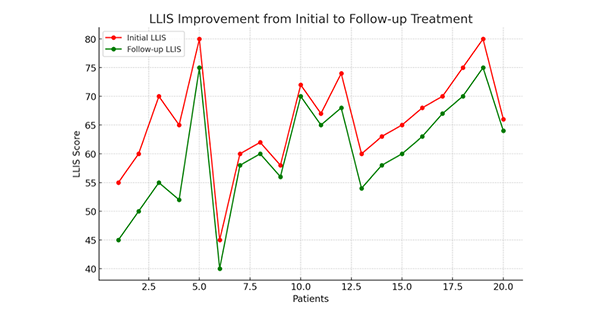
Patients reported significant improvements in their quality of life, with many stating that working with a local CLT enhanced their understanding of lymphoedema management. Feedback from patients, the healthcare team, and patient records revealed high satisfaction with the local service, which also resulted in better adherence to prescribed therapies and symptom control. Lymphoedema Life Impact Scores showed marked improvements, confirming the positive impact of the service.
The service included a comprehensive range of phase I complete decongestive therapy interventions, such as manual lymphatic drainage, compression bandaging, skin care, patient education, and exercise, with follow-up visits occurring five-times per week for 3–4 weeks to monitor progress and ensure proper compression garment fitting. During phase II of complete decongestive therapy (the maintenance phase), compression garment fittings and volumetric re-measurements were conducted every 6 months to ensure maintenance of optimal results. Overall, limb volume reductions by 10–30% were achieved, leading to decreased swelling and discomfort, which significantly improved patient outcomes.
Discussion
The establishment of lymphoedema services at NCH faced several challenges, primarily related to education, resource availability, and logistical constraints. While the medical team was proficient in general healthcare, there was limited familiarity with lymphoedema-specific treatment protocols. In-service presentations were conducted to enhance the understanding of lymphoedema and the unique needs of affected patients.
Additionally, the lack of a local medical supply store that works with patient insurance, compounded by the recent passage of the Lymphoedema Treatment Act, presented a significant barrier. To address this, a professional fitter travelled by ferry for some challenging sessions, and telehealth consultations were used to facilitate follow-up fittings. Many patients were unaware of the local lymphoedema community, which could have provided valuable peer support. Other logistical challenges, such as taking time off work for treatment and managing untreated skin conditions, further complicated care.
Volumetric measurements were taken using the traditional tape measurement method, which, while effective, can be more time-consuming and less accurate than advanced measurement technologies. In contrast, larger clinics off-island often utilise machines, such as the perometer, which employs infrared sensors to provide detailed, accurate limb volume measurements, or bioimpedance spectroscopy, which offers real-time data on tissue fluid levels and composition. These devices not only save time but also improve accuracy, facilitating better tracking of progress and adjustments in treatment. The absence of such technology in this remote setting has posed a challenge, limiting the potential for optimising treatment outcomes through more precise measurements.
Despite these barriers, the multidisciplinary team, which includes the CLT, local oncologist, nurses, primary care providers, and off-island specialists, worked in collaboration to ensure comprehensive care. The mentorship received from CLTs at Massachusetts General Hospital and Beth Israel Deaconess Medical Center was invaluable, helping to develop and refine care protocols. The introduction of a local CLT service has significantly improved access to care and patient outcomes, despite the challenges faced in this remote setting.
Limitations
While the new lymphoedema service has been effective in improving patient outcomes, challenges remain in increasing awareness and understanding of lymphoedema within the healthcare community, particularly among providers who are not specialized in this area. One key limitation is the lack of comprehensive lymphoedema education in medical curricula. Integrating lymphoedema management and recognition into training programs for medical students, nurses, and allied health professionals could help address this gap and ensure earlier identification and more effective treatment for patients. Additionally, the limited availability of advanced volumetric measurement technologies, such as perometers and bioimpedance spectroscopy, presents a barrier to achieving the highest level of accuracy and efficiency in monitoring patient progress. While traditional tape measurements are effective, they are time-consuming and less precise compared to these devices, which are commonly used in larger clinics.
Another limitation involves the logistics of obtaining lymphoedema garments and other necessary supplies. Patients had to wait for these items to be shipped from an off-island medical supply store, which typically took about two weeks. This delay added to the complexity of treatment and sometimes hindered timely interventions. Further research into the long-term effectiveness of remote service delivery, telehealth consultations, and the integration of advanced technology for measurements would provide valuable insights for improving service delivery and guiding future expansions of lymphoedema care.
Future Directions
In addition to fostering partnerships with medical supply companies, enhancing telehealth capabilities for remote follow-up consultations will improve patient access and reduce travel barriers. Long-term tracking of patient outcomes will also be essential to evaluate the effectiveness of the program. Developing a local support network for lymphoedema patients could help improve emotional wellbeing and encourage peer support. Collaboration with research institutions to further investigate the efficacy of lymphoedema treatments in remote settings could contribute to advancing care protocols. These initiatives will help ensure that services remain sustainable and effective.
Conclusion
The establishment of lymphoedema services at NCH has significantly enhanced patient access and dramatically improved health outcomes, demonstrating the power of localized care in remote settings. As the service continues to evolve, promoting its availability to the community through outreach and awareness campaigns will be crucial. With further investment in resources, telehealth expansion, and ongoing collaboration with off-island specialists, this initiative has the potential to serve as a model for similar underserved regions, ensuring sustainable, high-quality care for those in need.