Lymphoedema and manual lymphatic drainage (MLD) often emphasise volume reduction, but improvements in skin texture and the softening of adhesions are equally crucial. Up to 75% of head and neck cancer (HNC) patients who undergo radiotherapy exhibit lymphoedema symptoms. Additionally, the prevalence of psychosocial issues in these patients post-radiotherapy is estimated at around 63% (Nayak et al, 2022).
Lymphoedema involves the accumulation of protein-rich fluid in tissues, leading to swelling in various body regions, including the limbs, trunk, breast, head, neck or genital areas.
HNC patients undergoing radiation therapy often suffer from severe early and long-term side-effects, including permanent loss of saliva, osteoradionecrosis, radiation recall myositis, pharyngoesophageal stenosis, oral cavity necrosis, fibrosis, skin changes, lymphoedema and damage to neck structures. The likelihood and severity of these complications depend on various factors, such as the total dose of radiation, the duration of the treatment and the specific areas of the head and neck that received radiation. These side-effects present significant challenges to patients and their caregivers, necessitating lifelong strategies to mitigate their detrimental impact on basic life functions and overall quality of life. Conservative treatments, including lymphatic support through complete decongestive therapy, can be effective for managing fibrosis, lymphoedema and skin changes (Brook, 2020). Manual lymphatic drainage (MLD) is a widely accepted conservative treatment for lymphoedema. This case study investigates the efficacy of MLD combined with bioelectric massage therapy (BMT)/transcutaneous electrical nerve stimulation (TENS) for HNC patients post-radiotherapy. The use of non-invasive multi-modal treatments for managing lymphoedema can lead to volume reduction and significant improvements in swelling, skin texture and symptom-related outcomes in the affected areas and improved quality of life for HNC patients as is evidenced by this case study. During the study, patients also reported increased optimism about their condition, improved range of motion, ease in swallowing and speaking, increased saliva production, and reduced swelling. This study underscores the need for further experimental research on the effectiveness of MLD combined with BMT for managing lymphoedema in head and neck cancer patients.
Previous studies have demonstrated the benefits of MLD for limb reduction and quality of life improvement in lymphoedema patients (Williams, 2010). However, to date, no case studies have examined the effectiveness of MLD combined with bioelectric massage therapy (BMT)/transcutaneous electrical nerve stimulation (TENS) for HNC patients with lymphoedema.
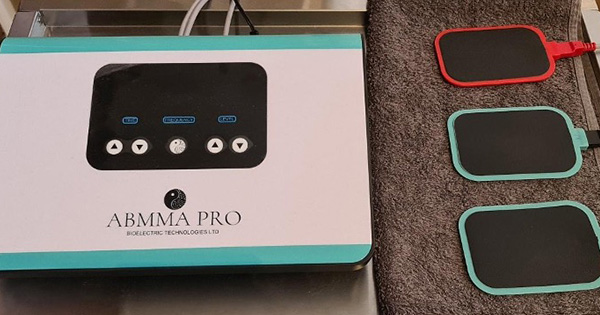
BMT uses a bioelectric device (ABMMA Pro; Figure 1) that generates a small electrical signal, which is transferred to the client’s body through the therapist’s hands. The ABMMA-Pro is a TENS device (TENS causes muscle contraction by stimulating α-motor neurons; Kang, 2015), but instead of using the pads as conduit, the therapist’s hands are the conduit. During the treatment, the therapist stands on a conducive mat (silicone mat with a damp towel and a conductive pad placed under the towel). A small current is transmitted via the therapist’s hands.
This case study explores the use of MLD combined with BMT in treating lymphoedema for a HNC patient post-radiotherapy.
Case presentation
A 66-year-old man with a history of total glossectomy, anterolateral thigh flap reconstruction and bilateral neck dissection presented with submandibular swelling, fibrosis and severely limited cervical mobility, impacting his quality of life, speech and swallowing (Figure 2).
Methods
For our sessions, we planned 45 minutes of bioelectric massage using the Casley-Smith (1992) method for MLD, following clearance of axillary nodes, sternal nodes, supraclavicular nodes and deep breathing technique.
Three sessions, each of 45 minutes duration, were scheduled, with one follow-up session. The initial three sessions were to be three consecutive sessions, each two days apart. The client was then asked to return for a follow-up session 13 days after the third session.
For this case study the day of the first treatment is referred to as day 1. The first three sessions were in close succession on days 1, 3 and 5, to take advantage of the cumulative effects of MLD with BMT.
The follow-up session was scheduled 13 days after day 5 (day 18).
For our sessions, we planned a course of treatment that would involve MLD with BMT, with the primary aim of reducing volume and circumference of neck as well as decreasing discomfort/pain and increasing range of movement.
The ABMMA Pro BMT device operates at two frequencies, high (50Hz) and low (12.5 Hz). Amperage can be controlled from level 1 to 40. For this case study, the low frequency at level 10 (4.53 mA) was used as we had used this frequency at a previous case study (Pluck, 2023)
A pad (the green pads in Figure 1) was applied with conductive cream on each of the patient’s upper lateral buttocks (gluteus medius).
Starting with the patient supine on the treatment table. Pressure was applied to supraclavicular nodes, followed by pressure to axillar nodes on each side. The patient then performed three diaphragmatic breaths after pressure was applied to his sternal nodes.
Using the bioelectric device, MLD was applied, using the Casley-Smith method. Massage started at the top of the axilla over the pectoral muscles, then the base of the neck and moving upwards to the ear but always in a downward direction (Figure 3), moving lymph towards the supraclavicular and sternal nodes. The gentle techniques used were to bring about changes in the tissue pressure and encourage lymphatic flow (Williams, 2010).
For the duration of the study, treatment was performed in the supine position only.
This course of treatment was expected to reduce the volume of the affected areas and increase the patient’s mobility.
Treatment regime
The treatment involved 45-minute sessions of bioelectric massage using the Casley-Smith (1992) method for MLD. The regime included three sessions scheduled over 5 days with a follow-up session 13 days after the third session. The ABMMA Pro BMT device was set to a low frequency at level 10 (4.53 mA), with conductive pads applied to the patient’s upper lateral buttocks (Pluck, 2023). The frequency chosen was previously chosen for a different case study and was well tolerated by this patient.
Response to treatment
Circumferential measurements of the neck were taken before and after each treatment while the patient was upright. Patient-reported outcomes, including pain levels (using the numerical rating scale 0–10), self-reported quality of life and mobility changes (photos), were recorded. Photographs documented pre- and post-treatment conditions (Figure 4).
Results
Subjective outcomes
Post-treatment, the patient exhibited increased range of motion, softened skin texture (this was observed by patient and therapists, although no actual measurements were taken), reduced tension in the tempero-mandibular joint, improved posture and ease in speaking. The patient’s optimism and continued self-management with regular MLD were also observed.
Objective outcomes
Despite no change in circumferential neck measurements (Figure 5), significant improvements in range of motion were noted (photos take pre- and post-treatments) and speech ability (patient reported and we were able to understand the patient better) were noted.
Discussion
This case study demonstrates how MLD combined with BMT can enhance musculoskeletal and psychological outcomes in an HNC patient with lymphoedema post-radiotherapy. Gentle MLD techniques and BMT-induced muscle contractions promote lymph movement and reduce pain and inflammation (Kim, 2014; Kang, 2015). These non-invasive treatments offer a viable alternative to more invasive methods, highlighting the need for personalised treatment plans and further research on their effectiveness.
Acknowledgements
This study was conceived and designed by Andrea Pluck and Jeremy Pluck. Data and investigation: Andrea Pluck and Jeremy Pluck. Photos and content used with patient consent. Revision and editing assistance: Greg Johnston.