Necrotising fasciitis (NF) is a soft tissue infection commonly caused by group A streptococcus (GAS) and is characterised by rapid progression and high mortality. It is considered one of the most dangerous infections in a surgical setting, as it remains silent for a long period and is diagnosed when it has already caused extensive local damage and systemic reaction. That means that early diagnosis is the most crucial step when dealing with this lethal condition, along with the formation of a multidisciplinary team that will be responsible for the patient during the whole treatment period.
Case report
A 47-year-old female and a user of a wheelchair for 18 years due to multiple sclerosis (MS) receiving teriflunomide (an immunomodulatory agent), came to the surgical accident and emergency (A&E), with sepsis as a result of an extended fourth-degree pressure ulcer in the sacrococcygeal region. Upon arrival, the patient was febrile (39oC) and hemodynamically unstable with a blood pressure (BP) of 80/40mmHg and a heart rate (MR) of 105 bpm. According to the 1-hour bundle for sepsis and septic shock, blood cultures and arterial blood gas were taken in parallel with the administration of broad-spectrum antibiotics (tazobactam, amycacin and clindamycin) and intravenous hydration. On clinical examination, the fourth-degree sacrococcygeal ulcer extended in the perirectal space, perineum, labia majora and continued until the upper inner surface of the right thigh. Laboratory studies showed that hematocrit was 25%, haemoglobin was 8g/dl, white blood cell count was 25,000, C-reactive protein was 21, sodium was 124 and lactate acid was 2.4. An immediate decision for her transfer to the intensive care unit (ICU) was made, where she was transfused, had correction of the electrolyte abnormalities and stated inotropic support with the aim of achieving a MAP >65mmHg. The patient remained there for a few hours to be stabilised before surgery.
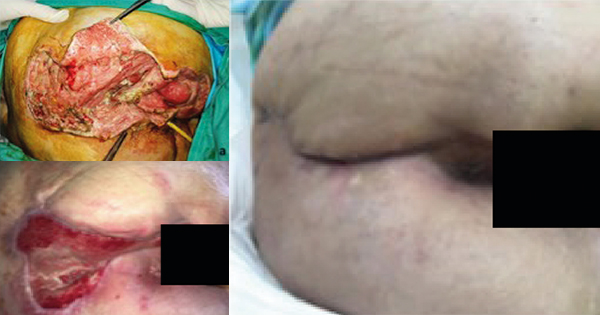
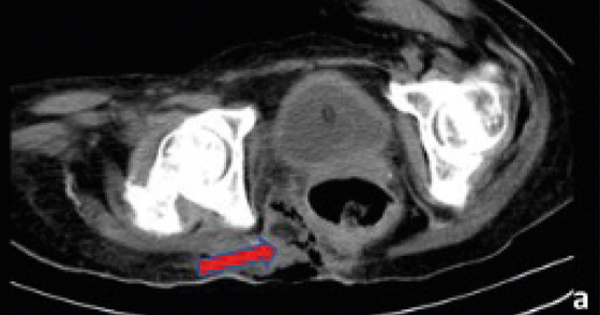
Following haemodynamic stabilisation, a computerised tomography (CT) of the upper and lower abdomen was performed, which showed perineal sepsis with pre-aortic and perirectal space inflammation and the presence of air in the soft tissues, without obstruction, perforation or other intra-abdominal pathology [Figure 1].
According to the Laboratory Risk Indicator for Necrotizing Fasciitis (LRINEC), the patient had a score of 9, indicating that she was at high risk for developing NF. All of the clinical and imaging findings were consistent with this diagnosis.
The patient was transferred to the operating room, where extensive surgical debridement of the wound was made [Figure 2a], followed by a bypass sigmoidostomy (trephine loop colostomy) without a laparotomy.
Postoperatively, surgical and mechanical wound debridements were performed in the operating room under general anaesthesia every 4–5 days, while in between, daily dressing changes were performed at the bedside. Sepsis was treated with antibiotics, initially empirically with daptomycin, meropenem, clindamycin and amikacin, and later based on the results of the blood, wound and tissue cultures. Results showed a polymicrobial infection with S. haemolyticus, S. epidermidis, Ac baumannii complex/S. haemolyticus*, Pseudomonas aeruginosa and Candida albicans, which was treated with piperacillin, fluconazole and amphotericin B.
The cultures were repeated after every debridement and dressing change and showed a changing profile of bacteria and resistances, so our patient was treated with ampicillin and ceftazidime until the day she was discharged. Despite the difficult anatomy of the area, Negative Pressure Wound Treatment (NPWT) was used, following the second surgical debridement.
In addition, nutritional assessment and support, as well as daily physical therapy and kinesiotherapy, were provided in order to prevent further complications related with reduced mobility and sepsis [Figure 2b]. The patient had to stay in the hospital for 90 days and during that period she had four surgical debridements under general anaesthesia and another 17 by the bedside. Despite the indications of improvement, it was decided to make early contact with the plastics department in order to accelerate recovery and rehabilitation. With the patient’s consent, clinical photographs and a summary of interventions so far were discussed with the head of the plastic surgical department of a major trauma hospital in Athens, as there is no plastic surgeon covering our hospital. Apart from his advice on the most appropriate wound care, he visited our hospital twice to evaluate the wound progression. Through collaborative weekly discussions, we developed a treatment plan, deciding that when the granulation tissue was healthy enough, he would perform a delayed closure at our clinic alongside our surgical team.
In addition, a tissue viability nurse (TVN) specialist was recommended in order to standardise the most appropriate method of NPWT application in such a difficult anatomical area. This multi-specialist approach accelerated wound healing and finally proceeded to reconstruction with skin advancement flaps. It was decided that this was the most appropriate method for two reasons: the progressive wound healing assisted by NPWT and the possibility offered by the area for mobilisation of the tissues and closure without tension. With an advancement flap, the closure of the wound was completed successfully [Figure 2c].
The patient was discharged on the 10th day after the reconstructive surgery, with instructions for dressing changes in the community and a weekly follow-up in the hospital. Figure 2d shows the result 2 months after the final intervention. Wound healing was completed without complications or recurrence and the patient is still symptom-free 3 years after the operation.
Discussion
NF is a severe and potentially life-threatening soft-tissue infection characterised by a rapid (and often silent) progressive necrosis of fascia and the subcutaneous tissue. The most common sites of infection are the lower extremities, abdomen and perineum (de Paula et al, 2019).
NF is associated with high mortality rates. Nordqvist et al (2015) found that the mortality rate was 19%, lower than other series of the past with fewer patients, but still quite high. NF is often associated with diabetes mellitus (Al-Qurayshi et al, 2020), as the prevalence has been reported to be between 44.5% and 72.3%. In contrast to common belief, it was found that the mortality rate among people with diabetes was 8.5%, in comparison with the 16.5% seen in those without diabetes. Other comorbidities that were also associated with high mortality rates were congestive heart failure, peripheral vascular disease, chronic liver disease and malignancy (Morgan, 2010).
Morgan (2010) also classified NF into four types based on the causative microbiological organisms: Type I (polymicrobial/synergistic pathogens), type II (monomicrobial and gram-positive pathogens) and type III (Gram-negative monomicrobial, bacterial infections from aquatic species and type IV caused by fungal pathogens). Almost 70% of cases are identified as type I, with most frequently identified pathogens group A streptococcus (GAS) bacteria. In our case NF was classified as type I because we had a polymicrobial infection with S. haemolyticus, S. epidermidis, Ac baumannii complex/haemolyticus*, Pseudomonas aeruginosa and Candida albicans.
Most of the time, patients present to the emergency room either complaining about a skin infection that is not improving despite antibiotics or upon arrival they are already in shock and have no idea what has caused them to be in this condition. As a result, early identification of NF is a major determinant of survival. However, studies have demonstrated that NF is often misdiagnosed as cellulitis or an abscess approximately 50% of the time, resulting in delayed intervention (Al-Qurayshi et al, 2020)
As early recognition is of paramount importance for a successful outcome, several clinical tools have been developed to address this. LRINEC is an easy tool, first described by Wong et al (2004), that we can use to raise our suspicion in cases presenting with the above clinical condition. A score of 6–7 indicates an intermediate risk, and a total score is >8, indicates a high risk. LRINEC should not be used alone to rule out NF. According to Fernando et al (2019), a LRINEC score equal to or over 6 has a sensitivity of 68.2% and specificity of 84.8%, while a LRINEC score equal to or over 9 has a sensitivity of 40.8% and specificity of 94.9%, while CT had a sensitivity of 88.5% and specificity of 93.3% (Fernando et al, 2019). For this reason, Bechar et al (2017) suggested a modified LRINEC, with the possible addition of clinical parameters, such as pain, pyrexia and comorbidities.
To our knowledge, our case is the first reported on a patient with MS receiving teriflunomide and NF. According to US Food and Drug Administration (FDA), teriflunomide can inhibit a key enzyme required by lymphocytes, reducing the proliferation of T and B immune cells active in MS and also inhibiting the production of immune messenger chemicals by T cells. It is not thought to affect resting immune cells that are not in an activated state. However, further research may be necessary to understand if there are any interactions with sepsis.
Early detection and surgical intervention was the first key to successful management of similar cases. As the patient arrived at the ER in an unstable state and had a high LRINEC score, immediate and adequate resuscitation and surgical intervention were performed without delay. The aim of surgical intervention is to remove all necrotic tissues along the muscle-fascial layers of the affected area until we reach healthy boundaries and achieve hemostasis (Zhao et al, 2017). Delays in the surgical debridement may be fatal, as the infection expands fast and it is crucial for the recovery of the patient to keep as many healthy tissues as possible.
Another factor that contributed to the positive outcome was the timely decision to perform a “second look” surgical intervention without any signs of deterioration, 48 hours after the first operation. Furthermore, at that early stage and despite the difficult anatomical region, we applied NPWT. NPWT provides several benefits to the wound; it keeps it clean by constantly draining and removing infected fluids, which reduces the size of the bacterial load. In addition, it eliminates extravascular oedema and improves microvascular blood supply, while at the same time, reinforcing the formation of granulation tissue and angiogenesis (Zhao et al, 2017; de Paula et al, 2019; Lee and Murray, 2020).
El-Sabbagh (2017) published a study on 41 patients treated with NPWT, including four cases with NF. As in this case, NPWT was applied immediately after debridement to prevent the formation of pseudo eschars and necrotic membranes that might necessitate more treatment. By adopting this technique, the general condition of the patient and the wound were dramatically improved.
A rare challenge faced in this case was that the perineum is a difficult area to apply NPWT due to the irregular surfaces created by the wound in close proximity to the labia, urethra and anus (Lee et al, 2012). The early stool diversion by a trephine loop sigmoidostomy in the first operation was critical to achieve a cleaner field and apply the NWPT. Furthermore, with the input of a TVN, we came up with a plan for regular changing of dressings every 72 hours with wound reassessment by the same team.
Even though surgical debridement and antibiotic agents are considered the main therapy of NF, Hyperbaric oxygen therapy (HBOT) and intravenous immunoglobulin (IVIG) therapy have been proposed as adjunct therapies (Al-Qurayshi et al, 2020). In our case, as the patient was improving and such additional treatments were not available, they were not used.
In addition to the individual steps, the authors believe that their team’s personal involvement with this patient’s care, involving the early involvement of a large multidisciplinary team harmonically collaborating for her care, was the major factor contributing to her recovery.
Conclusion
Necrotising fasciitis is a rare and complex disease, if not diagnosed at an early stage, can be fatal to the patient. A multidisciplinary, early and aggressive approach is fundamental for the survival of the patient. To our knowledge, this is the first case in the available literature involving patients with NF using teriflunomide, which could raise awareness about infective complications associated with immonomodulary treatments and lead to further research. In essence, the experience and co-operation of the several departments all contributed to this successful outcome. In the future, clinicians could be better trained to deal with and recognise such cases, reducing disease morbidity and mortality.