It is widely recognised that wounds are a common problem that affect individuals, the healthcare system and society as a whole (Moore et al, 2022). Living with chronic, complex or hard-to-heal wounds often results in a decrease in quality of life with the potential for increased pain and anxiety (Olsson et al, 2019). Opportunities to reduce this burden to patients, healthcare professionals and healthcare systems must be explored, and best practice must be incorporated into every patient’s journey.
Wound-related literature is awash with statistics outlining the financial burden of wound care. Every year, 420,000 patients in Australia suffer from chronic wounds (Australian Medical Association, 2022). According to Wounds Australia’s 2022 pre-budget submission, the annual cost to health and aged-care budgets was more than AUS$3 billion, with an average out-of-pocket cost to patients, who are mostly over 65 years old, of AUS$4,000 per year (Wounds Australia, 2022).
In Europe, an estimated 1.5 to 2 million people suffer from acute or chronic wounds, with approximately 15% remaining unhealed after one year (Lindholm and Searle, 2016). The estimated annual cost of wound management and associated comorbidities in 2017/2018 was £8.3 billion in the UK alone (Guest et al, 2020). Alarmingly, 25% of those wounds lacked a differential diagnosis and, all too often, inappropriate management compounds the problem. The mean patient care cost of an unhealed wound has been estimated at 135% higher than that for a healed wound.
This case series demonstrates the safe and effective use of PICO™ 14 Single Use Negative Pressure Wound Therapy System (sNPWT; Smith+Nephew, UK) in the management of static, hard-to-heal wounds when used in conjunction with optimal wound care strategies, including patient empowerment and education.
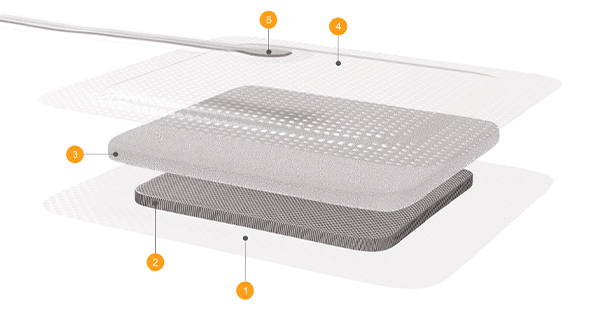
It is imperative to recognise that negative pressure (both traditional and single use application) is a therapy, not a passive dressing. Its mode of action includes delivering increased blood flow, reducing local tissue oedema and removing fluid and bacteria from the wound bed (Schwartz et al, 2015). Negative pressure has the potential to actively treat the wound rather than simply manage the symptoms (Schwartz et al, 2015). In a recent study, this brand of sNPWT system and dressing showed superiority versus traditional negative pressure in managing chronic lower-extremity wounds, demonstrating greater reductions in wound area, faster re-epithelialisation and increased quality of granulation tissue (Kirsner et al, 2019). It has been shown that sNPWT delivers negative pressure across a wider area than just the wound itself, administering consistent compressive forces to surrounding tissue, which may benefit perfusion and management of oedema (Casey et al, 2019) [Figure 1].
A higher level of patient satisfaction was reported in the sNPWT group versus traditional negative pressure across several parameters including comfort, impact on sleep, impact on mobility and willingness to use again in the future (Kirsner et al, 2019). Unlike most traditional negative pressure systems, its portable design is ideal for patients at home or people who do not want their mobility restricted (Hudson et al, 2015).
Hard-to-heal wounds can be defined as wounds that develop due to an interruption in the body’s natural healing process (Hampton et al, 2022) and fail to heal with standard therapy in an orderly and timely manner (Vowden, 2011). Common, interchangeable terms for ‘hard-to-heal wounds’ include stalled, static, non-healing and chronic, with ‘hard-to-heal’ now being advocated as a more positive and patient-friendly description (Fletcher et al, 2022).
These wounds, regardless of how they are referred to, are challenging to treat, with associated costs consistently falling on budgets outside secondary care. Hampton et al (2022) published encouraging results when they utilised sNPWT to manage chronic wounds in the community setting, with 52% healed in a mean of 6.3 weeks. However, the likelihood of healing decreased from 63% for wounds present for less than 6 months to 28.4% for wounds present for over a year, adding strength to the argument for proactive treatment plans.
Many factors contribute to failed or stalled healing (Wounds UK, 2018; Fletcher et al, 2022) [Table 1]; a proactive approach and recognition of the potential barriers are imperative to healing early in the treatment cycle. Current best practice advocates the importance of considering which factors can be easily modified, are slow to be modified or cannot be modified, so that implementation of local and systemic care delivery offers patients improved yet realistic outcomes (Fletcher et al, 2022).
Improved healing observed in patients with wounds of less than 6 months in duration (Hughes et al, 2021) emphasises the importance of early and proactive intervention to have a positive impact both on the patient experience and associated health economic outcomes.
A holistic assessment is integral to all patient care. The phrase ‘holistic wound assessment’ emphasises a requirement for a comprehensive assessment that considers the impact of all aspects of the patient’s health and wellbeing on the healing process, helping to avoid the pitfall of focusing only on the wound (Wounds UK, 2018). In 2018, a group of wound experts convened and concluded that patients with one or more wounds should receive a holistic wound assessment, a concept that is now accepted as best practice (Wounds UK, 2018). This involves identifying factors that require intervention and developing treatment objectives or goals of therapy as well as guiding appropriate patient care and wound management (Wounds UK, 2018).
The COVID-19 pandemic forced a transformation in ways of working globally, increasing opportunities for practitioners to explore the adoption and wider standardisation of shared care. Patients, who were previously passive recipients of service provision, are now encouraged and educated on how to participate in care planning and delivery of their care (Moore et al, 2021). A cross-sectional study concluded that patients with type 2 diabetes have the potential to be empowered to manage their chronic disease if they are actively informed and educated (Tol et al, 2013). Likewise, Moore et al (2021) proposed that effective patient involvement cannot be achieved unless the patient gains the necessary knowledge and skills and is educated about their condition.
Wound care encompasses many indications, with a plethora of underlying pathologies that contribute to their development. For example, without a differential diagnosis and strong patient engagement to treatment, healing rates of venous leg ulcers (VLUs) can be catastrophically affected (Wounds UK, 2019). Early and accurate diagnosis, patient empowerment and engagement and a proactive approach by the healthcare provider are widely accepted as evidence-based approaches to achieving successful outcomes, improving patient quality of life and reducing financial burden.
This case series of four patients [Table 2]depicts the exceptional results that can be achieved when a holistic, proactive approach is combined with sNPWT.
Case 1
An 88-year-old man presented with an unstageable pressure injury/pressure ulcer (PI/PU) to his left heel which developed 24 weeks prior to initial specialist assessment [Table 3]. Medical history included congestive heart failure, atrial fibrillation and osteoarthritis. Formerly mobile with a frame, the patient was rendered chair/bedbound due to the wound. Nutritional intake had diminished and was recorded as inadequate. Previous treatment consisted of daily topical application of povidone iodine lotion and foam dressings.
Wound bed was obscured by 100% black eschar [Figure 2]. Sharp debridement, performed to deliver wound bed preparation, revealed friable wound edges, a moderate amount of purulent exudate and a distinct malodour. [Figure 3] Pain levels using numeric pain intensity scale were described as significant with a score of 10/10. Table 1 specifies the factors required for holistic patient-centred treatment.
sNPWT with gauze filler was selected to provide homeostasis, manage exudate and encourage granulation tissue formation. Skin protectant was applied to surrounding tissues. After one week of therapy, the distal aspect of the wound was sharply debrided further and sNPWT was reapplied without the use of gauze filler. A reduction in pain was reported, now at 4/10. Within 3 weeks, healthy granulation tissue and reduction in wound size were evident [Figure 4]. The patient tolerated sNPWT well, with no adverse events. Complete closure of this chronic wound was achieved in 42 days [Figure 5], allowing the patient to regain mobility and return to his hobby of bowling.
Case 2
A 48-year-old male with complex medical history, including quadriplegia, rapid atrial fibrillation, history of sepsis and hypertension was admitted to hospital for surgical debridement of a deteriorating category IV pressure injury [Table 4]. As an inpatient, he successfully received 4 weeks of RENASYSTM traditional negative pressure wound therapy (tNPWT). Following discharge, treatment comprised of moistened gauze, absorbent dressing and fixation tape. Significant wound deterioration occurred requiring specialist intervention.
Holistic assessment revealed alarming non-concordance with pressure area management, including prolonged wheelchair use. Despite utilisation of a pressure-reducing support surface, such prolonged periods without offloading were considered detrimental to healing potential. The wound bed was red with moderate levels of haemoserous exudate, but there was no pain or odour reported [Figure 6].
This time using sNPWT was considered the most appropriate treatment plan to support homeostasis, manage exudate and promote wound closure but also facilitate independence and mobility while using a wheelchair, which is imperative to a young and independent patient. Prior to applying sNPWT with gauze filler for 14 days, SECURA™ wipes (Smith+Nephew, UK) were used to clean the surrounding tissues.
By day 12 of sNPWT, healthy granulation tissue filled the wound bed and sNPWT was continued without the use of gauze filler and applied by general nurses[Figure 7]. A seal was easily attained and maintained with no reported issues. The care package included reinforcement and education about optimal nutritional intake and pressure area management requirements. sNPWT was discontinued at day 28 when total closure was achieved [Figure 8]. To reduce the risk of future pressure damage, ongoing support with pressure area redistribution, skincare and psychological support will be required for the rest of the patient’s life.
Case 3
A 66-year-old female presented with a VLU that had been present for 6 years prior to referral [Table 5]. An extensive past medical history including hypertension, hypercholesterolaemia, cerebral vascular accident, atrial fibrillation and depression, resulted in more than 12 different medications being taken. The patient previously worked as an administrative assistant. Dressing leakage due to excessive exudate resulted in a leave of absence from work and social isolation. Her poor mobility and unsteady gait made her vulnerable to trauma and disturbed wound healing.
Historically, multiple treatments were prescribed by different general practitioners (GP) and nurses including most recently, InadineTM dressing (3M/KCI, USA) changed three times per week by her GP. The patient’s non-concordance with best practice, such as compression therapy and elevation of legs, exacerbated the problem. Consequentially, the wound deteriorated and, at 3cm deep, required hospitalisation. tNPWT was commenced, and following improvement, the patient was discharged home on foam dressings and a crepe bandage, with a GP referral to the Consultant Nurse.
The wound bed displayed deep red, unhealthy tissue, exuding moderate levels of haemoserous fluid, but there was no odour or pain reported. Wound edges were macerated with dry skin to the lower limb [Figure 9]. Differential diagnosis of VLU.
Active therapy was considered the most appropriate option with sNPWT being selected. After 6 days of sNPWT, size reduction was visible and at 12 days, granulation tissue appeared healthy with islands of epithelial tissue were evident in the wound bed. Instigation of sNPWT appears to be the pivotal point at which the wound responded and a positive healing trajectory ensued[Figure 10]. Total wound closure was achieved in only 29 days post-initiation of sNPWT, facilitating a return to normal life [Figure 11]. Unfortunately, at no point was compression therapy considered by the patient, therefore future recurrence is a real risk. A skincare regimen of twice-daily SECURA barrier cream (Smith+Nephew, UK) was implemented to address dry lower limbs.
Case 4
A 58-year-old female had surgical pins and plates implanted to address a crush injury in her right foot [Table 6]. Past medical history included soft tissue pain (post-accident), eczema, diminished learning capacity and moderate chronic arthritis (left knee). As an inpatient, multiple dressing regimens were instigated without success, and she was discharged from hospital with a foam adhesive dressing and a prognosis of chronic lifelong wound. A GP referral was made to a consultant nurse for specialist advice.
The patient presented with a non-healing wound on the lateral aspect of their foot, oedema present, a pink wound bed and minimal serous exudate [Figure 12]. There was no odour and the pain experienced at dressing change was reported as 5/10. The patient was unable to attend her usual place of work which exacerbated challenging behaviours.
Microdacyn™ spray (Te Arai BioFarma, Australia) was prescribed as an antimicrobial treatment and 14-day sNPWT was initiated. Wound closure was the ultimate goal; however, a poor prognosis was noted. After 12 days of sNPWT, there was visible improvement and size reduction [Figure 13]. By day 24, closure of the tissues was achieved [Figure 14]. Nevertheless, it is recognised that recurrence rates in such wounds are high, requiring strict vigilance regarding footwear, skincare and investigation into suitability of compression hosiery. Healing this wound enabled the patient to return to her volunteer work, providing psychological stability and an improved quality of life.
Conclusion
NPWT has increasingly been seen as an enabling technology for moving suitable patients out of high-cost acute care hospital environments and into their homes (Hudson et al, 2015). sNPWT has demonstrated superior results in open wounds (Kirsner et al, 2019 ) and, because of its size and portability, lends itself to use in a community setting for patients requiring independence.
This real-world evidence depicts a group of patients ranging in age, case complexity, wound type and wound longevity. Prior to specialist intervention, these wounds were chronic and showed no signs of improvement. The use of sNPWT in conjunction with holistic assessment, proactive treatment, patient education and patient-centred care enabled all wounds to heal and patients to achieve an acceptable quality of life.
New guidance has been developed outlining ways in which to support practitioners, particularly in the community, to improve the care of patients with non-healing wounds. This may be challenging in some settings; however, it is hoped that by defining best practice and the processes required to implement it, practitioners will be encouraged to make organisational changes that will benefit patients with non-healing wounds (Wounds UK, 2022). It is the responsibility of each practitioner to review, modify and evaluate their practice in order for these urgently needed changes to occur.