Complex and complicated wounds (CCWs) are a common challenge for clinicians. Despite increased knowledge, wound care innovations and best practices implemented, wound healing is often prolonged. Non-healing wounds easily get infected, causing complications like amputations and even sepsis (Calis et al, 2020). This affects patients psychologically, and increases financial burdens for healthcare systems and patients (Vowden et al, 2008).
Causes of delayed wound healing include:
- 1) Prolonged inflammatory stage
- 2) Failure of normal growth factor synthesis,
- 3) Overexpression of protease activity,
- 4) Increased disintegration of growth factors due to lack of normal anti-protease inhibitor mechanisms (Barbul et al, 2015; Calis et al, 2020).
When any of these occur, the activities of matrix metalloproteinases (MMPs) get dysregulated (Caley et al, 2015). This disturbs degradation and deposition of the extracellular matrix; a process crucial for wound re-epithelialisation.
Advanced wound care aims to facilitate wound progress to the proliferative phase of wound healing. In clinical practice, wound management should incorporate evidence-based literature with advanced wound therapies. One such advanced wound therapy to manage CCWs is NPWT (Calis et al, 2020).
Negative pressure wound therapy
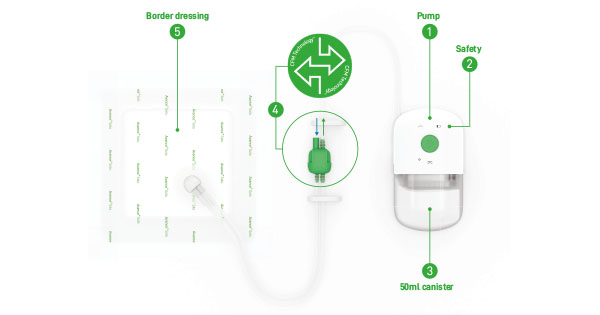
In 1997, Morykwas et al described Negative pressure wound therapy (NPWT) as “placing an open-cell foam dressing into the wound cavity and applying a controlled sub-atmospheric pressure”. In his observational study, 98.7% of wounds responded significantly, with increased blood flow levels, granulation tissue and random-pattern flap survival, and decreased tissue bacterial count (Morykwas et al, 1997).
Application of constant negative pressure induces a physical response (macrostrain) and a biological response (microstrain). Macrostrain draws wound edges together, removes exudate and infectious materials, reduces oedema and promotes perfusion. Microstrain creates tissue micro-deformation and stretches cells, causing cell migration and proliferation, inducing granulation (Vellingiri and Hongaiah, 2020).
Nano-oligosaccharide factor (sucrose octasulfate) contact layer dressing based on technology lipido-colloid (TLC-NOSF)
Nano-Oligosaccharide Factor (NOSF) possesses matrix metalloproteinases (MMP)-reducing properties. Furthermore, it has been shown in numerous publications to promote healing in various wounds (Richard et al, 2012; White et al, 2015).
Technology Lipido-Colloid (TLC) comprises a matrix containing hydrocolloid and lipophilic substances. (McGrath et al, 2014). Upon contact with wound exudate, this matrix converts into a lipido-colloidal gel, creating a moist wound healing environment and promoting granulation (Bernard et al, 2005; 2009).
In a 2021 systematic review on sucrose octasulfate dressing (TLC-NOSF), 21 publications of different levels were identified, ranging from double-blind randomised control trials (RCT) to case reports, some involving over 12,000 patients. They showed that TLC-NOSF dressings: i) are an evidence-based option for management of chronic wounds, ii) promote healing processes, reduce healing times and enhance patients’ health-related quality of life, and iii) are more cost-effective in general (Nair et al, 2021).
The complex and complicated wound
The patient was a 59-year-old Chinese male with longstanding type 2 diabetes with ensuing retinopathy, hypertension, hyperlipidaemia, peripheral vascular disease (PVD) and end-stage renal failure (ESRF) on haemodialysis. In 2013, he was diagnosed with coronary artery disease with triple vessel disease, paroxysmal atrial fibrillation and non-ST-elevation myocardial infarction (NSTEMI). In 2020, the patient underwent left lower limb (LL) angioplasty with triple vessel flow below the knee to the foot achieved.
The patient first presented to the emergency department on June 1, 2021 with wet gangrene of the first right toe. A first right ray amputation was performed the next day, followed by a right lower leg angioplasty on 4 Jun with completion outflow of anterior tibial artery only. Subsequently, due to wound deterioration, a right forefoot amputation was performed on June 10, and NPWT with instillation (NPWTi) of normal saline initiated the following day. On 18 June, a collagen dressing was introduced to cover exposed metatarsal bones in the wound bed. Thereafter, the patient underwent two rounds of surgical debridement on 29 June and 27 July. The wound bed was still unhealthy after three weeks, with 70% slough and 30% granulation.
Towards the end of August, the patient was discharged home with a NPWT machine without instillation. This continued for 2 months, with a 2 weeks pause in October, where the wound was dressed only with gauze and a collagen dressing packed into its cavity in the first week and silver alginate dressing in the second week. Albeit by October 25, the wound size was 8 x 4.3cm, undermining by 1.8cm, extremely exudative, with heavy periwound maceration. Patient was restarted on home NPWT with collagen dressing. After two weeks, only slight progress was noted. The wound size was 7.5 x 4.5cm, still undermining by 1.8cm.
The hypothesis
Previous studies have identified that when used as an interface layer between NPWT foam and wound bed, TLC dressings reduce “the size of wounds faster … without reducing the effectiveness of negative pressure therapy” (Baek et al, 2020). NOSF also reduces healing time in complicated wounds (Nair et al, 2021).
In a double-blind, multi-centre RCT conducted across European countries in 43 hospitals (Explorer study), TLC-NOSF dressings demonstrated efficacy in healing of acute and chronic wounds of differing wound durations (Lázaro-Martínez et al, 2019). Within 20 weeks, irrespective of wound duration, patient group using TLC-NOSF dressings exhibited a 60% increase in wound closure versus group using control dressing (Edmonds et al, 2018).
An open label 12-week, two-arm, multicentre, randomised study comparing TLC-NOSF dressing to collagen oxidised regenerated cellulose (CORC), a type of collagen dressing showed a mean difference of 33.6 ± 15.0% for percentage wound relative reduction in favour of TLC-NOSF, with a unilateral 95% confidence interval lower limit of 8.6% (excluding null value; Schmutz et al, 2008). A superiority of the effectiveness of TLC-NOSF as compared with CORC was concluded (p=0.0059 for superiority test).
The author hypothesised that inclusion of TLC-NOSF dressing as an interface layer with NPWT would enhance healing in a wound not responding well to NPWT. This new treatment regime was initiated on the above case on 8 November.
Wound progress after TLC-NOSF dressing
Healthier granulation tissue and wound size reduction were noted during first dressing change on 11 November [Figure 1]. This persisted over time [Figure 2] and by week 14, wound size had reduced by 87.5%, with zero depth [Figure 3]. NPWT was discontinued, and wound was dressed with TLC-NOSF dressing and silicon border foam dressing.
By 1 June (week 29), wound had almost completely healed [Figure 4]. Although wound healing took considerable time, progress of wound after initiation of TLC-NOSF dressing was remarkable. It was concluded that there was significantly improved healing, evidencing the hypothesis proposed. The author decided to test this out on other cases to further substantiate hypothesis.
The cases
Case 1: A 37-year-old Chinese male with longstanding type 2 diabetes, ensuing retinopathy, maculopathy, ESRF on haemodialysis, hypertension, percutaneous coronary intervention and PVD.
He first presented to emergency department on September 23, 2021 with wet gangrene of the left first toe. He underwent left first toe disarticulation, LL percutaneous old balloon angioplasty (POBA) and stenting of superficial femoral artery (SFA) on 29 September, and surgical wound debridement on 10 October, 27 October 27 and 1 November. He commenced NPWT on 11 October 11, and hyperbaric oxygen therapy on 20 October.
After six weeks the outlook for the wound remained bleak. Thus, the patient underwent surgical wound debridement of the left first toe disarticulation wound on 15 December, left second ray amputation on 17 December, left forefoot amputation, a repeated LL POBA with CFA endarterectomy, iliac and SFA stenting on 29 December, and further cutback of wound on 3 January, 2022. NPWTi with hypochlorous acid solution was initiated on January 4. 17 days after forefoot amputation, wound size was 7.6 x 5.5cm, with all metatarsals exposed and 1st metatarsal loose. There was only some granulation.
Consequently on 26 January, patient underwent another left LL angioplasty and Lisfranc amputation. After two days, the wound bed was largely granulating with cuneiforms and cuboid exposed and multiple areas of silver nitrate staining and cauterisation [Figure 5]. Wound size was 7.8 x 5cm, with adipose tissue on plantolateral aspect of wound bed and thick adherent fibrin on plantar medial aspect of wound. Home NPWT was initiated with TLC-NOSF dressing as an interface layer.
One month later, significant wound progress was noted [Figure 6] with improvements in wound size by 29.9%. Wound bed was 70% granulating (with healthy granulation over bone), and 30% sloughy. Wound continued to progress with decreases in size, improved wound appearances and lesser non-viable tissue over the weeks. By week 15, the wound had improved in size by 83.8% [Figure 7], showing remarkable wound progress in spite of the patient’s poor medical condition, vascular status and prognoses.
Unfortunately, the patient developed a left heel wound which rapidly became wet gangrene, and underwent a left below knee amputation (BKA) on 22 May.
Case 2: A 55-year-old Indian male with longstanding type 2 diabetes, ensuing retinopathy, cataract, hypertension, hyperlipidaemia, PVD, ischaemic heart disease (more than 50% stenosis) and NSTEMI.
The patient first discovered a blister on his left lateral heel on 9 April, 2022, which developed into a wound shortly after. On 12 May, he was referred to the podiatrist. Toe pressure was borderline (67mmHg on left first toe). Non-viable tissue was debrided and wound dressed with a silver dressing.
By 30 May the wound had deteriorated, with increased depth and necrotic slough. The patient was referred to the vascular surgeon, and underwent an elective left LL angioplasty (POBA) on 17 June with completion outflow of posterior tibial and peroneal arteries. Three days later, wound became infected with exuding pus and malodour. The patient was readmitted and underwent surgical debridement on 22 June. On 24 June, the wound bed was granulating with 2 spots of slough. NPWTi with hypochlorous acid solution was initiated, with TLC-NOSF dressing placed over wound as an interface. Wound size was 3 x 3.7cm, with a depth of 1.5cm [Figure 8].
After four days the wound showed good progress and was granulating with 30% of slough. Patient was discharged home, on home NPWT machine with TLC-NOSF interface layer. By 10 day, the wound size had improved by 44.1%. The wound bed was granulating with fibrin overlying.
By week 7, the wound had improved in size by 52.1%, with only slight fibrin overlying the granulating wound bed [Figure 9]. NPWT was discontinued. TLC-NOSF dressing was used on the wound together with a silicon border foam dressing. The wound continued to progress well and by week 18, wound size had improved by 99.3% [Figure 10]. Wound size was 0.2 x 0.4, and depth was 0.3cm.
Discussion and conclusion
Wounds characterised by an abnormal sequence of wound healing processes often result in complications that regulate the delay and development of lingering wounds (Bassetto et al, 2022). CCWs are often multifaceted, making treatment tremendously difficult, and posing a significant challenge for many healthcare providers (Tricco et al, 2015). Comorbidities contributing to delayed wound healing include limited vascularity in PVD, metabolic disease, immunosuppression, peripheral neuropathy, chronic medications and connective tissue disease (Bassetto et al 2022). Clinicians ought to use interventions backed by evidence, and tailor them in an effective manner to suit their patients’ needs (Tricco et al, 2015).
The author first encountered a CCW in August 2021 that did not progress well despite good standards of care. Strong evidence on the efficacy of TLC-NOSF dressing in wound healing was found (Nair et al, 2021) and, thus, the author came out with the hypothesis that inclusion of TLC-NOSF contact layer dressing in the management of the wound would contribute to wound healing.
This hypothesis was trialled on the CCW, with encouraging results observed, and further confirmed in two other cases where good outcomes were similarly attained. TLC-NOSF dressing has since been used with and without NPWT on other wounds of varying durations in Chinese, Indian and Malay patients with similar positive outcomes.
Although this paper describes use of TLC-NOSF dressing in Asian cases in a Singaporean context, results are favourable and mirror the positive results from European studies used in Nair et al’s systematic review in 2021. This suggests equal efficacy of TLC-NOSF dressing in: i) both acute and chronic wounds, ii) an Asian population, and iii) patients of different racial groupings. Additional trials should be conducted to validate this hypothesis.
Furthermore, TLC-NOSF dressing has demonstrated robust impacts in accelerating wound healing and closure in younger wounds, as seen in the complete healing of 71% of wounds of less than 2 months duration versus only 22% of wounds more than 11 months duration, within 20 weeks (Edmonds et al, 2018). We therefore recommended the initiation of evidence-based treatments, such as TLC-NOSF dressings, as soon as possible, so as to reduce and even prevent the progression to CCWs.