According to the latest version of the Consensus Document of the International Society of Lymphology (2023) for the evaluation and management of peripheral lymphoedema, an accurate diagnosis of lymphoedema is essential for effective treatment. It is based on clinical history, physical examination and tests, such as lymphoscintigraphy, MRI, bioimpedance, ultrasound, indocyanine green fluorescence and others. Lymphoedema is classified based on a linear severity scale from 0 to III, and its management requires an interprofessional approach, as it affects physical, mental, social and financial health. Conservative treatment focuses on the following approaches: manual lymphatic drainage, compression bandages and stockings, therapeutic exercises and skin care, among other approaches. Among the gaps identified by the International Society of Lymphology, the lack of randomised clinical trials with robust methodology, validation of lymphatic biomarkers, development of more accurate assessment scales, digital technologies for remote monitoring and public policies and large-scale professional training stand out (International Society of Lymphology, 2023).
Traditional health education methods include lectures, printed materials, and group training for self-bandaging. However, insufficient information on specialised professionals and products often hinders long-term adherence to care routines. Factors such as lack of motivation, financial constraints, and forgetfulness contribute to poor disease management (Vignes et al, 2017; Ligabue et al, 2019; Omidi et al, 2020; Peter et al, 2021; Ciudad et al, 2024).
Accessible self-management tools in clear language are needed to improve communication between healthcare professionals and patients, enhancing self-care, empowerment, and monitoring. Despite their importance, health-related applications, particularly for lymphoedema, are scarce in Portuguese, are not fully functional and not free of charge(WHO, 2021).
In the digital age, the use of artificial intelligence (AI) has also been increasingly used in health-related advances such as lymphoedema. A recent article by Mangion (2024) presented the results of a case study of a lymphoedema professional who used Bard (Google’s generative AI brand) and ChatGPT (OpenAI’s brand) to differentially diagnose lymphoedema and lipoedema, based on the following symptoms: specific bilateral symptoms and leg pain. The author concludes that neither of the two generative intelligences used provided conclusive information for a differential diagnosis of lymphoedema and/or lipoedema, reinforcing that professionals trained in lymphoedema need to rely on their own training and have a high level of understanding of specific oedemas to be able to correctly diagnose their patients while further AI research is enabled, as technology continues to evolve and learn from the responses.
As lymphoedema is a global health issue with significant physical and psychological consequences, this study aimed to develop a mobile application that provides accessible support and guidance, empowering patients in managing their condition.
Material and methods
This study was approved by the Research Ethics Committee of the Universidade Federal de São Paulo (UNIFESP), Brazil (CAE 58037722.0.0000.5505). Written informed consent was obtained from all patients prior to their inclusion in the study; patient anonymity was assured.
To create and build the application, the design thinking (DT) method was used, and four stages were applied: discover (desk research), define, develop and deliver (Ferreira et al, 2015).
Desk research was carried out through a systematic literature review. The terms Mesh and its synonyms (“Lymphedema AND Mobile Applications”) were used. The search was carried out in the databases: LILACS, PubMed, SciELO, Google® and Google Scholar®. To evaluate the relevance of the topic and conduct preliminary research, a search was performed on the Apple Store and Google Play platforms for smartphone apps, as well as on Google for web apps, using the keywords “mobile application” and “lymphedema.
The analysis of articles and information was conducted to address three questions:
- What problems do the questionnaire respondents face?
- What methods do the study participants currently use to try to solve these problems?
- What can be done to improve the situation faced by the questionnaire respondents?
Interview
Thirty individuals aged 18 years or older, diagnosed with secondary lymphoedema in the upper or lower limbs and having undergone treatment, participated in the study. A questionnaire (Google Forms® link via WhatsApp®) assessed their needs in four key areas: lymphoedema management, information, daily care and available resources.
In the define stage, patient challenges were analysed. The develop stage, following the Double Diamond framework, involved five brainstorming sessions between researchers and an IT technician. Application formats and functionalities were selected based on survey responses and literature review. The Dema app was designed in collaboration with Slide Works, with screen mock-ups created in PowerPoint®. Prototyping used Figma® for web-based design and interface testing.
During the deliver stage, a Figma®-recorded video of the prototype was shared via WhatsApp® for participant evaluation. A follow-up questionnaire (Google Forms®) assessed usability, navigation, improvement suggestions, and willingness to pay, using a 3-point Likert scale (2=high, 1=medium or 0=low).
Participant ratings and feedback were evaluated and used as a basis for fine-tuning the app. After evaluating the interviewees, a diagram of the tool was created with the complete content of the final application.
Based on the results, the creation of the application went through the following steps:
- The programming language used was React Native, a JavaScript library created by Facebook®. It is used to develop applications for Android® and iOS® systems natively.
- Subsequently, accounts were created in digital application stores for mobile devices following the standards applied by each of them: Apple Store and Google Play to upload the application.
The application for patients with lymphoedema is available free of charge on the website of the professional master’s degree in science, technology and management applied to tissue regeneration at Unifesp and in the Apple® and Google Play® stores.
Results
During the desk research, articles were collected that addressed learning, self-management and the use of tools related to lymphoedema with a view to adapting the material to the development of the application.
The literature on lymphoedema management highlighted four most relevant topics, which were compiled and described as: “Lymphedema Management”, “Lymphedema Information”, “Lymphedema Daily” and “Lymphedema Resources”.
The review of the literature on mobile applications for lymphoedema identified a few studies specifically using mobile applications for this disease.
Figure 1 illustrates the articles found in the search with the outcome tools for managing lymphoedema.
Table 1 presents the main topics of articles published in the specialised literature on the use of applications for lymphoedema.
In addition to the desk research, a preliminary search was also carried out for applications on Android and iOS mobile devices, identifying their main characteristics. These articles are also listed in Table 1.
A Questionnaire was applied for the interview. Thirty-eight invitations were sent, of which 30 were considered for analysis and eight were excluded, six for not accepting/signing the informed consent form and two for answering the questionnaire incorrectly, invalidating it. In total, 30 individuals responded to the questionnaire, only one of whom was male and the rest female. Below, in Table 2, are the main results found after the interview.
The results of the “discover” phase were presented, the objectives of the study and the results after the application of Questionnaire 1, which highlighted the “management” category as the most relevant. The interest in behaviours that help self-management, maintaining routine care to control lymphoedema and psychological support for these patients defined the lack of support and access to these essential guidelines for self-management of lymphoedema.
After brainstorming sessions between the researchers and the IT technician, and based on the answers to the questionnaires and the desk survey from the discover phase, the characteristics and content of the lymphoedema management theme were developed and included in the prototyping.
We took the opportunity to discuss a name for the application, and “Dema” was chosen – a derivation of the word lymphoedema, as well as the creation of a logo/icon that identifies the application.
The icon that identified the application was inspired by a lymph node and presented different-sized extremities, representing the effect that lymphoedema can have on the patient’s body.
In this prototyping, user identification tabs (name, age, gender and location of lymphoedema) and management tabs were created. In the management tab, the following sub-tabs were included: data for the day (number of steps, amount of water intake, perimetry, skin hydration and exercise log), guidance and care (elevation, massage, exercise, compression, hygiene and medicine ), muscular strength and daily activities (questions for self-assessment of muscular strength and carrying out daily activities), limb protection (use of gloves and boots, repellents, appropriate clothing, sunscreen), exercises and therapies to do at home (videos with illustration of self-massage, self-wrapping, exercise, and use of compression stockings).
After the prototyping was completed, contact was resumed with the study participants to deliver and evaluate the prototype through multiple-choice questions. Of the 30 patients, 27 presented themselves for the evaluation and application of Questionnnaire 2. Table 3 presents these responses.
The suggestions analysed through open questions that asked about improvements and use of the application were considered and included in the final version of the application.
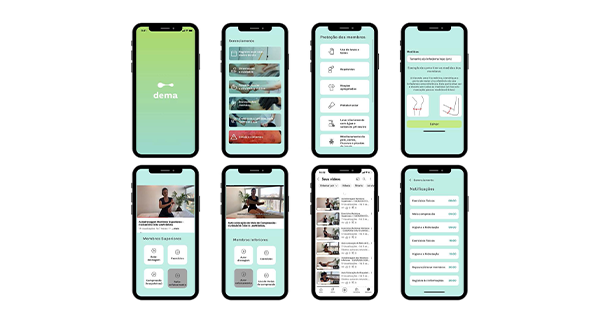
Figure 2 illustrates the interfaces and layout of the Dema application functions. The final version of these interfaces considered the comments and suggestions from study participants, which were evaluated jointly by researchers and application developers. Thus, a notification tab was inserted, which reminds/notifies the user of the care and activities to be carried out during the day, as well as highlighting the signs and symptoms sub-item, with a more striking colour and illustrative figure, denoting attention. More care was also added to the limb protection tab.
The application is published and available free of charge on the website of the professional master’s degree in science, technology and management applied to tissue regeneration at Unifesp and the Apple and Google Play stores.
Discussion
With DT, the primary challenge for lymphoedema patients was identified: the lack of support and guidelines for disease management. The Dema app was developed to address this need, aligning with literature findings emphasizing the importance of self-management in preventing disease progression and maintaining quality of life (Fu et al, 2016; Douglass et al, 2016; International Society of Lymphology Executive Committee, 2023; WHO, 2023).
Participants identified management (63.3%) as the most relevant app feature, including daily care, exercises, reminders, and self-monitoring. While existing health apps focus on isolated aspects such as exercise or volumetric calculation, Dema integrates multiple self-management tools, offering comprehensive guidance based on gold-standard treatments.
Given the limitations that made it difficult to group and analyse data (different samples studied, different characteristics and outcomes in each application surveyed in the literature), as well as the creation of an application centred on the need and perception of patients with lymphoedema to manage their condition, a solution was created that was aligned, through the patient’s interest, in managing their health condition. The Dema app, in particular, was created for Android and iOS, with features enabled (ready to use). Furthermore, the objective was to prevent the worsening of lymphoedema, reducing inflammatory crises, medical complications, loss of mobility and functionality through management and daily monitoring of basic care, hygiene, and exercise.
Accessibility was a priority, considering technological literacy, aging populations, and regional factors. The app’s design included clear fonts, intuitive navigation, and illustrations for quick information retrieval. A usability questionnaire revealed that 52% of participants were willing to pay for the app, though alternative funding models (e.g., government or private sector support) were suggested.
The use of “Dema” not only provides accessibility in terms of costs for obtaining the application, but also helps to reduce travel costs, increase patient adherence to self-management care, and reduce expenses related to the need for specialist professionals, as met by the information contained in the application. These aspects were highlighted in the studies by Omidi et al (2020) and Okutsu and Koiyabashi (2014).
Future enhancements include other functionalities, such as 3D volumetric calculation, monitoring graphs and alerts for critical signs and translation into other languages, as more patients use it and can contribute through the evaluation of the tool, including your practical needs, also combining the monitoring medical clinic and its evaluation parameters. Furthermore, other healthcare professionals and companies specializing in lymphoedema products will also be able to contribute to an impactful tool that meets the needs of the Brazilian population with lymphoedema and its characteristics. There is the prospect of a future study that proves the reliability and validity of using Dema in patients with lymphoedema.
Conclusion
“Dema”, a mobile application offering accessible support and guidelines for patients diagnosed with lymphoedema, was developed. The application empowers patients to take a central role in self-managing their condition.