In 2019, the International Diabetes Federation (IDF) reported that over 77 million individuals have diabetes in India, which will increase to over 100 million by 2030 (IDF, 2019). Of these people with diabetes, 25% will develop a diabetic foot ulcer (DFU), equating to 5 million by 2030. Overall, half of ulcers become infected during the healing process, necessitating hospitalisation, while 20% of these patients require amputation. DFUs contribute to approximately 80% of all non-traumatic amputations performed annually in India (Ghosh and Valia, 2017). It is indicated that social epidemiology regarding DFU in India differs from the West due to many factors including socio-economic and cultural factors. This can lead to significant delay in specialist referral, with patients still relying on treatment based on local ethnic methods and not based on scientific data. This results in patients presenting with highly infected ulcers (Rastogi and Bhansali, 2016).
Infections in wound management are closely associated with delayed healing, increased complications such as amputation, and, moreover, have a negative impact on patients’ quality of life (Cutting, 2016; Armstrong et al, 2017). Furthermore, due to the complications that ensue, infections can increase the economic burden on healthcare facilities related to wound management and increase hospital stay (Nussbaum et al, 2018). The overall management plan for people with DFUs (and for that matter any chronic wound) should include six spheres: mechanical control or pressure offloading, medical/metabolic control of the diabetes and comorbidities, microbiological/infection management, vascular control ensuring adequate blood flow, wound control and education aimed at increasing patient awareness of foot care over their lifetime.
Management of wound infection needs to include understanding and involvement of the patient’s response and the local wound healing environment, as well as a reduction of the microbial load as part of the standard of care. This will include wound cleansing, debridement, and appropriate use of topical antimicrobials (International Wound Infection Institute, 2016).
The use of technology lipido-colloid with silver (TLC-Ag) is supported by high-quality clinical evidence in the management of wounds at risk or presenting with clinical signs of local infection; TLC-Ag dressings show superior efficacy in reducing wound bioburden, while also promoting wound healing. Additionally, results demonstrate high tolerance and acceptability of TLC-Ag dressings because of their atraumatic properties (Lazareth et al, 2007; 2008; Schäfer et al, 2008; Lazareth et al, 2012; Allaert, 2014). TLC-Ag dressings with cohesive poly-absorbent fibres (UrgoClean Ag) have been developed to manage wounds with higher levels of exudate and trap sloughy residues and can be used throughout the stages of wound healing (Meaume et al, 2012; 2014; Dissemond al, 2020).
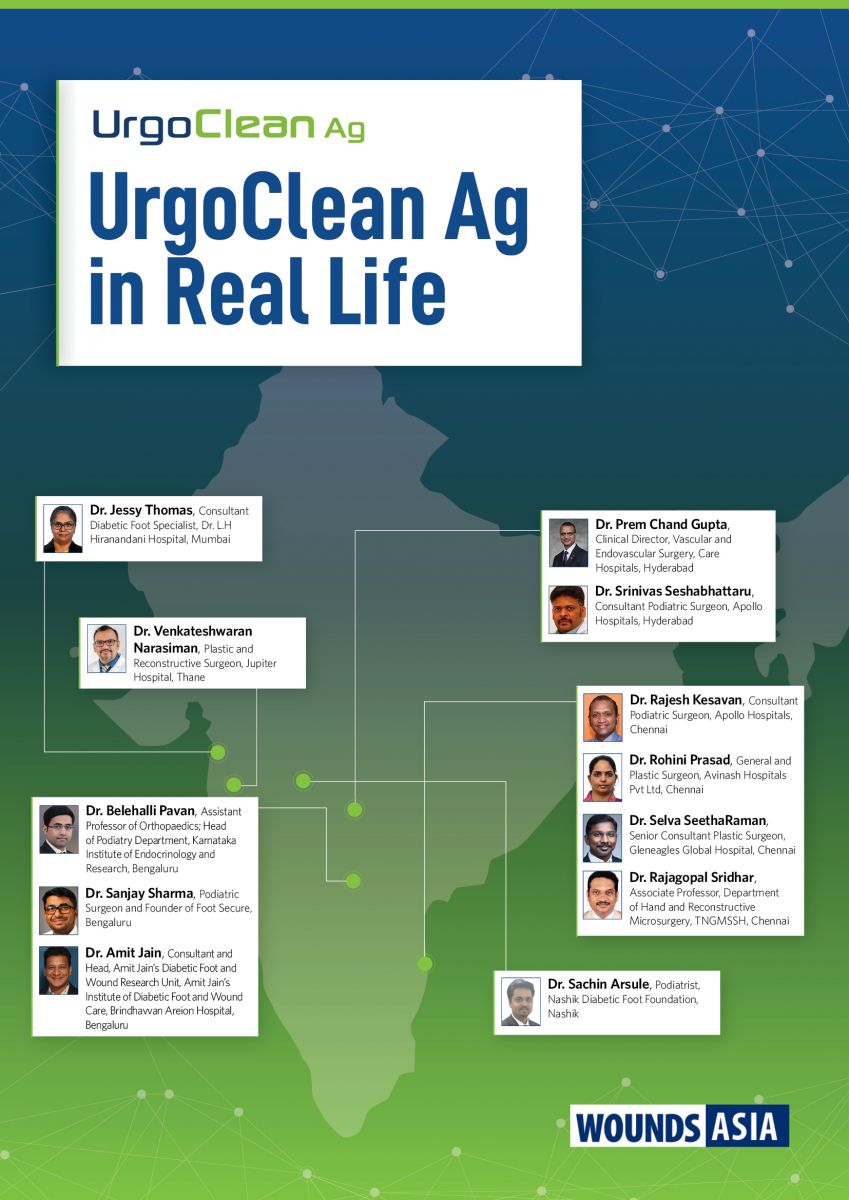
This document showcases the outcomes of UrgoClean Ag in a real-world environment, demonstrating enhancement in the management of DFU in India with improvement in wound conditions and, furthermore, enhancing the patients’ quality of life and clinicians’ satisfaction. Clinicians and organisations worldwide need to understand that appropriate wound management interventions based on high-level evidence should be used to formulate local guidelines and DFU care pathways.
Dr. Srinivas Seshabhattaru, Consultant Podiatric Surgeon