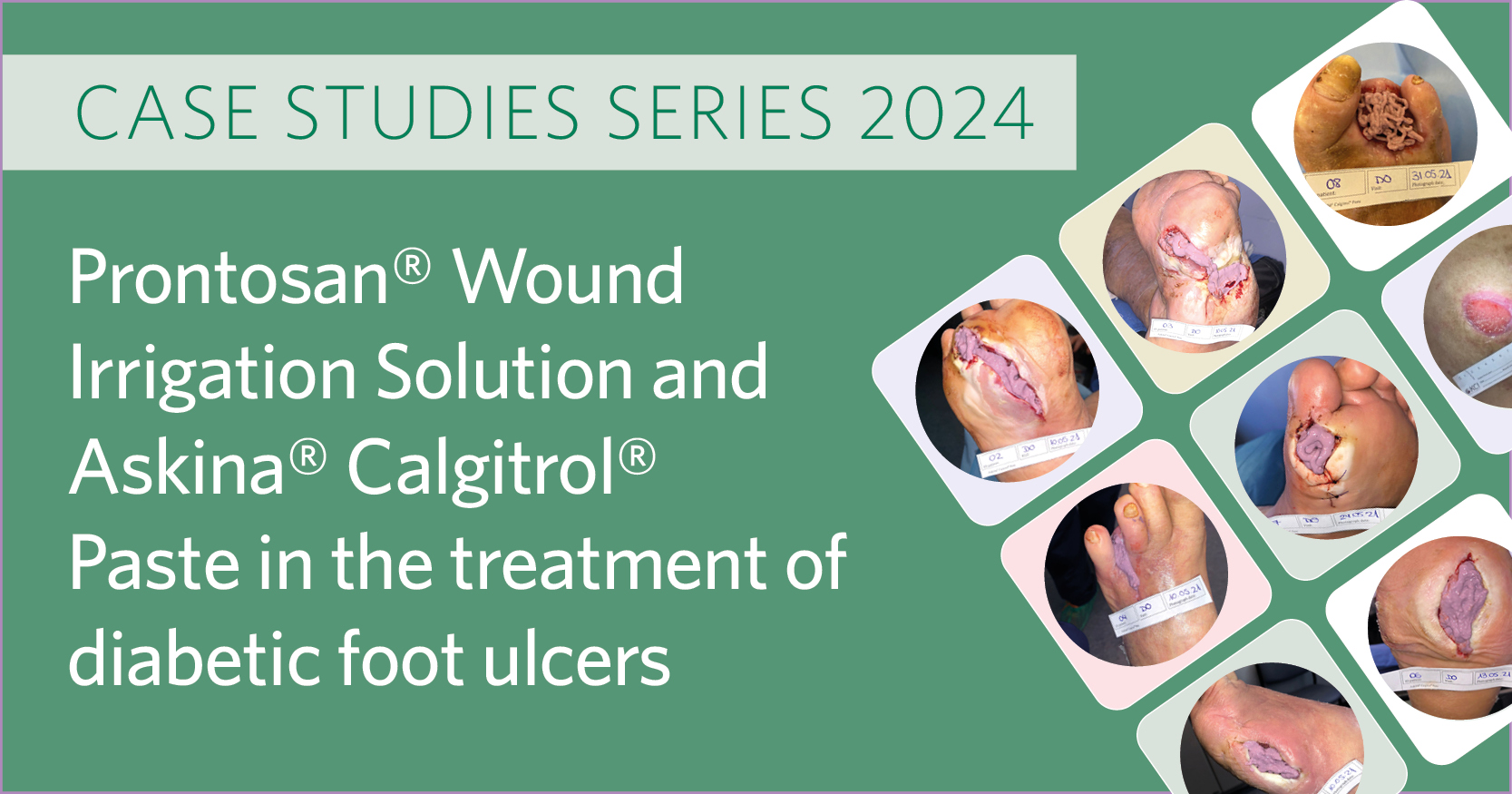
The prevalence of wounds is increasing globally, particularly in the Asia-Pacific (APAC) region. The International Diabetes Federation (IDF) estimates that there were 537 million people with diabetes worldwide in 2021, and up to one-third of those individuals will experience a diabetic foot ulcer (DFU) during their lifetime (Nair et al, 2022). The high prevalence of diabetes in the APAC region accounted for over 60% of the 5.1 million deaths caused by diabetes globally in 2013 (Organisation for Economic Co-operation and Development [OECD],2020). In Australia, there are 400,000 people affected with chronic wounds, which is associated with a direct healthcare cost of AUD$3 billion (Australian Centre for Health Services Innovation et al, 2017). This equates to 2% of the Australian national healthcare expenditure. On pressure ulcers alone, it is estimated that AUD$983 million is spent annually and more than 500,000 bed days are lost. While official statistics are either unavailable or difficult to access in the APAC region, a comprehensive population-based analysis in Singapore between 2000 and 2017 estimated that among all Singaporeans hospitalised for acute care, the incidence of wounds was 300 per 100,000 adults over the age of 18 and 800 per 100,000 adults over the age of 50 (Goh et al, 2020).
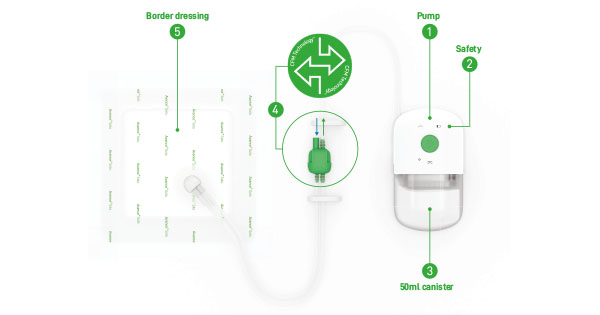
Negative pressure wound therapy (NPWT) is the gold standard treatment for many open acute and chronic wounds (Bakaeen et al, 2019; Kim and Kang, 2020; Seidel et al, 2020). NPWT involves applying the NPWT system to a dressing that is designed to deliver suction and promote wound healing. There are two general delivery systems — traditional negative pressure wound therapy (tNPWT) and single use negative pressure wound therapy (sNPWT).
The use of tNPWT can be complex and resource-intensive and hospital resources may struggle to match the growing demand. There are hidden costs that can increase the economic burden associated with using NPWT and discharge processes are complex (Kirsner and Hurd, 2020; Hurd et al, 2021). As a result, an international panel of 5 clinicians from Malaysia, Singapore, Australia and New Zealand with experience in wound care and NPWT developed a set of recommendations to help povide optimal patient care and resource efficiency. The panel aimed to advise clinicians on when to consider NPWT use in acute and chronic wound management and provide a practical decision-making tool, known as the OneNPWT clinical decision tree for open wounds, to guide on NPWT modality (RENASYS™ Negative Pressure Wound Therapy System or PICO™ Single Use Negative Pressure Wound Therapy System) and when it should be used.
This case series describes how the OneNPWT decision tree was used in clinical practice by wound care specialists in the APAC regions. The decision tree was used within local protocol to prompt initiation of either RENASYS™ tNPWT or PICO™ sNPWT. Each patient was monitored and reviewed until NPWT was ceased or until full wound closure. The characteristics of the wounds (i.e. size, wound bed composition) were recorded at dressing change.