Wound exudate is a fundamental part of wound healing, but if it is present in the wrong amount, location, composition, or consistency, it can cause complications, such as infection and damage the periwound skin. This may lead to maceration increasing the wound surface area and prolonging healing time (Haryanto et al, 2016; World Union of Wound Healing Societies [WUWHS], 2019).
Wound exudate contains a variety of components, including a high level of proteases that degrade proteins (e.g. matrix metalloproteinases [MMPs]), micro-organisms, substances that can inhibit healing, as well as proteins that promote the growth of bacteria. This leads to an increased risk of infection and subsequent development of biofilm (Young, 2012).
If exudate is not effectively managed, exudate can pool at the base of the wound bed. The risk of exudate pooling increases when dead space or a ‘gap’ forms as a result of the dressing not maintaining direct contact with the wound bed. The gap presents a clinical challenge as the increased risk of exudate pooling leads to an increased risk of leakage, maceration, and infection, which may delay wound healing (Cutting et al, 2009; Young, 2012; Haryanto et al, 2016). Highly exuding, sloughy and cavity wounds, wounds with undermining and wounds with a steep angle between the wound edge and wound bed, and fistulas are at a higher risk of dead space and exudate pooling (Dowsett et al, 2019; von Hallern et al, 2020).
Gelling fibre dressings
Gelling fibre dressings are a solution for moderate-to-highly exuding wounds (WUWHS, 2019) and are a well-accepted treatment option in the management of exudate. Upon exudate absorption, the fibres form a gel that supports autolytic debridement and tissue granulation, and helps maintain a moist wound environment (Dabiri et al, 2016).
However, challenges remain when using gelling fibre dressings (Karlsmark et al, 2020):
- Not all gelling fibres are effective at absorbing and retaining large amounts of exudate, which can lead to complications
- Some gelling fibre dressings have a surface shrinkage of more than 36% upon wetting (NHS, 2018), which can lead to gap formation, exudate pooling and maceration
- Clinicians can often experience issues in removing gelling fibre dressings, such as the dressing breaking on removal or leaving residue or debris in the wound, which leads to increased time being required to remove the dressing or deal with resultant issues.
Biatain® Fiber with HexaLock Technology
Biatain Fiber (Colopast) with HexaLock Technology is a soft gelling fibre dressing with integrated strength, which effectively absorbs and retains large amounts of exudate. The dressing keeps its shape with minimal shrinkage, thereby minimising the risk of gap creation and reducing exudate pooling. Biatain Fiber can be easily removed in one-piece with minimal risk of leaving residue in the wound. (Karlsmark et al, 2020; Garcia Dominguez et al, 2021; Le et al, 2021).
The benefits of Biatain Fiber are enabled by HexaLock Technology, which is a combination of three components: an optimised combination of absorbing carboxymethylcellulose (CMC) gelling fibres and strengthening fibres; thermobonding that locks the fibres together; and a hexagon net applied by ultrasonic embossment.
Biatain Fiber is intended for use as a primary wound dressing for use in highly exuding, sloughy and cavity wounds, including undermining. It is available in a square or ribbon variant and can be cut to fit the size of the wound.
The choice of secondary dressing will depend on the characteristics of the wound. Covering Biatain Fiber with a conforming foam dressing, such as Biatain® Silicone with 3DFit Technology (Coloplast) can provide additional vertical absorption in highly exuding wounds.
Clinical experiences using Biatain Fiber
The experiences of clinical groups in Italy and Spain using Biatain Fiber on various types of wounds were presented at the European Wound Management Association Conference 2021 (De Angelis et al, 2021; Blasco et al, 2021). In both posters that included five patients, the dressing supported wound healing very well. The dressing had high absorption and retention capacity, managed high viscosity exudate and protected the wound edges and periwound skin from maceration.
A recent survey exploring the opinion of clinicians in Spain on performance of the new reinforced gelling fiber confirmed that satisfaction with Biatain Fiber was high. From 399 responses, clinicians particularly valued the following properties of Biatain Fiber (Garcia Dominguez et al, 2021):
- The exudate management capacity = Absorption was evaluated as ‘very good’ or ‘good’ in 99% of the evaluations and retention was evaluated as ‘very good’ or ‘good’ in 97% of the evaluations. In an open-ended question on the greatest benefits of the dressing, 74% of the evaluations specifically mentioned benefits relating to exudate management.
- The ability to debride the wound = Debridement capacity was evaluated as ‘very good’ or ‘good’ in 83% of the evaluations.
- The ability to keep its shape with minimal shrinkage = Level of shrinkage was evaluated as ‘very good’ or ‘good’ in 97% of the evaluations, and 93% stated that it is ‘very positive’ or ‘positive’ to have minimal shrinkage in a fiber dressing.
- The ability to remove the dressing with ease and without leaving a residue = No residues were left in the wound was reported in 85.2% of the evaluations.
- The ability to remove the dressing in one piece = In 99% of the evaluations, the dressing could be removed in one piece.
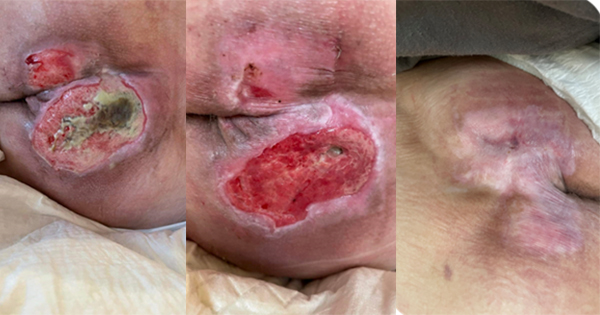
Case study evaluations
Here, we present nine cases evaluating the clinical performance of Biatain Fiber dressing on various types of wounds. The Triangle of Wound Assessment (Dowsett et al, 2019) was used by the clinicians to assess and manage all areas of the wound – the wound bed, wound edge and the periwound skin. The Triangle of Wound Assessment guides clinicians to undertake a holistic assessment, set management goals and select the optimal treatment for the patient and wound.
The patient and wound were regularly monitored for clinical signs of improvement, such as reduction in wound size; improvement in wound bed tissue composition and periwound skin condition; reduction in exudate levels and malodour; signs of infection; and impact of the wound on patient quality of life. Any relevant additional treatment and advice were also reported, such as pressure offloading, debridement, secondary dressings and periwound skin care.
Cases 1 and 2 are ulcers related to diabetes, cases 3 and 4 are burns, case 5 and 6 are abdominal surgical dehisced wounds, case 7 is a sacral pressure ulcer, case 8 is a heel pressure ulcer, and case 9 is a venous leg ulcer. These cases are representative of a clinician’s everyday use of Biatain Fiber dressings.