What is Wound Balance and how does it help clinicians manage complex wounds?
Wound Balance is a concept integrating all relevant factors to ensure continuity and personalised care, guiding clinical decision-making and addressing the imbalances contributing to wound complexity or chronicity (Wounds International, 2023).
Wound Balance [Figure 1]emphasises a holistic approach that helps clinicians identify and remove the barriers to healing—offering insight into why certain wounds become complex and, ultimately, non-healing (WUWHS, 2025).
Achieving optimal healing outcomes requires identifying the three categories of wound healing barriers [Figure 2].
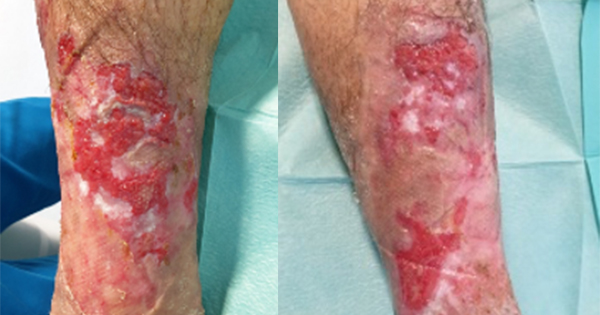
Are wounds complex or non-healing?
The inconsistency in terminology can be confusing for clinicians and may carry negative connotations for patients; for example, “failed to heal wound” suggests to the patient that the wound will likely never heal. Not all complex wounds become non-healing or chronic; however, they all require prioritised care. Since every non-healing, chronic wound begins as a small wound, early intervention is essential to prevent complications and promote optimal healing.
WUWHS recommendation: Wound Balance requires that clinicians assess all wound and patient-related factors as per patient’s needs in the particular clinical setting, and identify the barriers to healing.
Use of consistent language and terminologies can help achieve better outcomes for patients and assist clinicians in providing timely interventions. Previously, these wounds have been referred to as ‘non-healing’.
WUWHS recommendation: The consensus panel agreed wound chronicity definitions should be revisited and encouraged the use of the term ‘complex wounds’ .
The WUWHS-recommended tools for achieving Wound Balance
Early identification of risk factors and accurate assessment
The TIMERS framework was recommended by the WUWHS panel—Tissue, Infection/Inflammation, Moisture, Edge, Repair/Regeneration, and Social—as a means to enable timely and effective intervention [Box 1; Lumbers, 2019]. In addition to evaluating the wound bed, TIMERS incorporates social factors that may affect a patient’s quality of life (QoL) and healing. As such, it offers a holistic approach that supports the integration of Wound Balance into everyday clinical practice (Lumbers, 2019; National Library of Medicine [NLM], 2025).
Timely and consistent intervention with Superabsorbent Polymer (SAP) dressings
When aiming to achieve Wound Balance, practical measures should be taken to reduce factors that inhibit healing, including consistent and appropriate removal of excessive exudate (which contains healing inhibitors) or bacterial load, while keeping the wound and peri-wound protected.
Reducing wound care complexity
The WUWHS panel found the Wound Balance concept intuitive, noting it helps reduce complexity often associated with wound care. Wound Balance clarifies dressing selection, particularly when aligning with other treatments such as compression therapy. The panel members expressed a preference for using a single dressing type to support healing and highlighted that SAP dressings restore the trajectory of wound healing [Figures 3-5].
Debridement
Wound debridement is a clinical technique that aims to convert a complex, non-healing wound environment to an acute wound environment, supporting the progress of healing (WUWHS, 2025).
The consensus panel highlighted how often clinicians working in primary care/community settings may not be trained or allowed to safely undertake sharp debridement, and that autolytic debridement (e.g. via hydro-responsive wound dressings [HRWDs]) may be the most appropriate option for their patients. HRWDs hydrate the wound, allowing for autolytic debridement [Figure 5]. The Wound Balance concept will assist clinicians to align patient goals and clinical needs (e.g. reduction of necrotic tissue, bioburden and/or inflammation).
The WUWHS recommendations on achieving Wound Balance with SAP dressings
Through evidence collected via case studies, the WUWHS panel shared their own clinical experiences of applying Wound Balance via SAP dressings (recommendations summarised in Figures 3-5). SAP dressings are applicable for all wound aetiologies, in all clinical settings and throughout the wound healing trajectory, providing the following benefits:
- Less frequent dressing changes required (continuity of treatment may also improve patient satisfaction
and engagement) - Control of healing inhibitors (e.g. matrix metalloproteases)
- Improvement of the patients’ QoL
- Patients staying in work
- Improvement of life activities
- Increased patient engagement
- Improved financial benefits for patients due to less dressing changes and reduced number of prescriptions required.
The consensus panel noted that, in their experience, SAP dressings [Figures 6-8] offer an effective solution for wounds not requiring urgent review. The high absorbency and ease of use prevent maceration, resulting in fewer dressing changes. This, in turn, contributes to cost savings and reduces the need for daily clinic visits.
The panel also emphasised the importance of using SAP dressings alongside compression therapy. As low-
exudate wounds can become wetter once compression begins—leading to discomfort and reduced patient adherence—SAP dressings help manage exudate effectively and enhance patient comfort.
Improving QoL outcomes using Wound Balance
Enhancing a patient’s QoL is fundamental to achieving Wound Balance. Individuals with non-healing wounds often encounter daily challenges that disrupt their routine activities and mental well-being (Wounds International, 2023). Reduced mobility, pain and the distress caused by exudate leakage and malodour can lead to social isolation, anxiety, depression and disengagement from care (Olsson et al, 2019; Zhu et al, 2022). As such, QoL-focused interventions are central to delivering truly balanced, patient-centred care (Wounds International, 2023).
With its effective, holistic and affordable treatment options, Wound Balance can help patients achieve these goals.
WUWHS recommendation: The panel recommended that patients experiencing social isolation or lack of access to appropriate wound care should receive suitable education so they can successfully manage self-care and achieve healing
Effective communication with patients
The clinical care aspect of Wound Balance helps clinicians prioritise decision-making parameters while keeping the patient central to all interventions. The WUWHS panel emphasised that healthcare professionals must ensure patients are informed, involved and provide clear consent throughout assessment
and treatment.
WUWHS recommendation: Education should be provided through easy-to-use resources, both verbally and in print, encouraging patients to confirm their understanding.
With its holistic, practical and cost-effective approach, Wound Balance supports patients in reaching successful healing outcomes.
Benefits of implementing Wound Balance
Incorporating the Wound Balance concept into daily practice allows clinicians to shift the wound to a healing state. SAP dressings support this early intervention through their specific mechanism of action, addressing the imbalance of critical biomarkers which, in excess, act as wound inhibitors.
Summary
Implementing Wound Balance at an early stage via evidence-based interventions, such as the SAP dressings, is an achievable goal in routine care to improve healing, reduce clinician time and is cost-saving due to reduction in dressing use. Recommended by the WUWHS experts [Figure 9], the Wound Balance concept assists clinicians to align patient goals and clinical needs (e.g. reduction of necrotic tissue, bioburden and/or inflammation) and has been shown to improve patient outcomes across all wound aetiologies and all clinical settings (WUWHS, 2025).
Download the PDF below to access the full Made Easy resource.